Role of Ramadan Fasting on Secretory IgA and Statherin Levels in Individuals with Dental Caries
DOI:
https://doi.org/10.32007/jfacmedbagdad.6622252الكلمات المفتاحية:
Dental Caries، Fasting، Gingival Index، Plaque Index، Secretory immunoglobulin A (sIgA)، Statherinالملخص
Background: Tooth decay happens when bacteria in the mouth create acid from carbohydrates that can be fermented. Along with factors related to the person (like genetics or oral hygiene habits) and saliva, this process leads to cavities. During Ramadan fasting, when eating habits change, there could be effects on health, particularly on the salivary biomarkers that are important for dental well-being.
Objectives: This cross-sectional study aimed to detect the activity and concentrations of salivary levels of secretory immunoglobulin A and Statherin during and after Ramadan fasting and to evaluate the association between these biomarkers with dental caries.
Methods: The study comprised 40 individuals, aged 20-25 years, diagnosed with dental caries. Participants were assessed for periodontal parameters using the Plaque Index and the Gingival Index. Saliva samples were collected during the fourth week of Ramadan fasting and two weeks after Ramadan fasting. The concentrations of both secretory IgA and Statherin were measured in salivary samples using Enzyme-Linked Immunosorbent Assay .
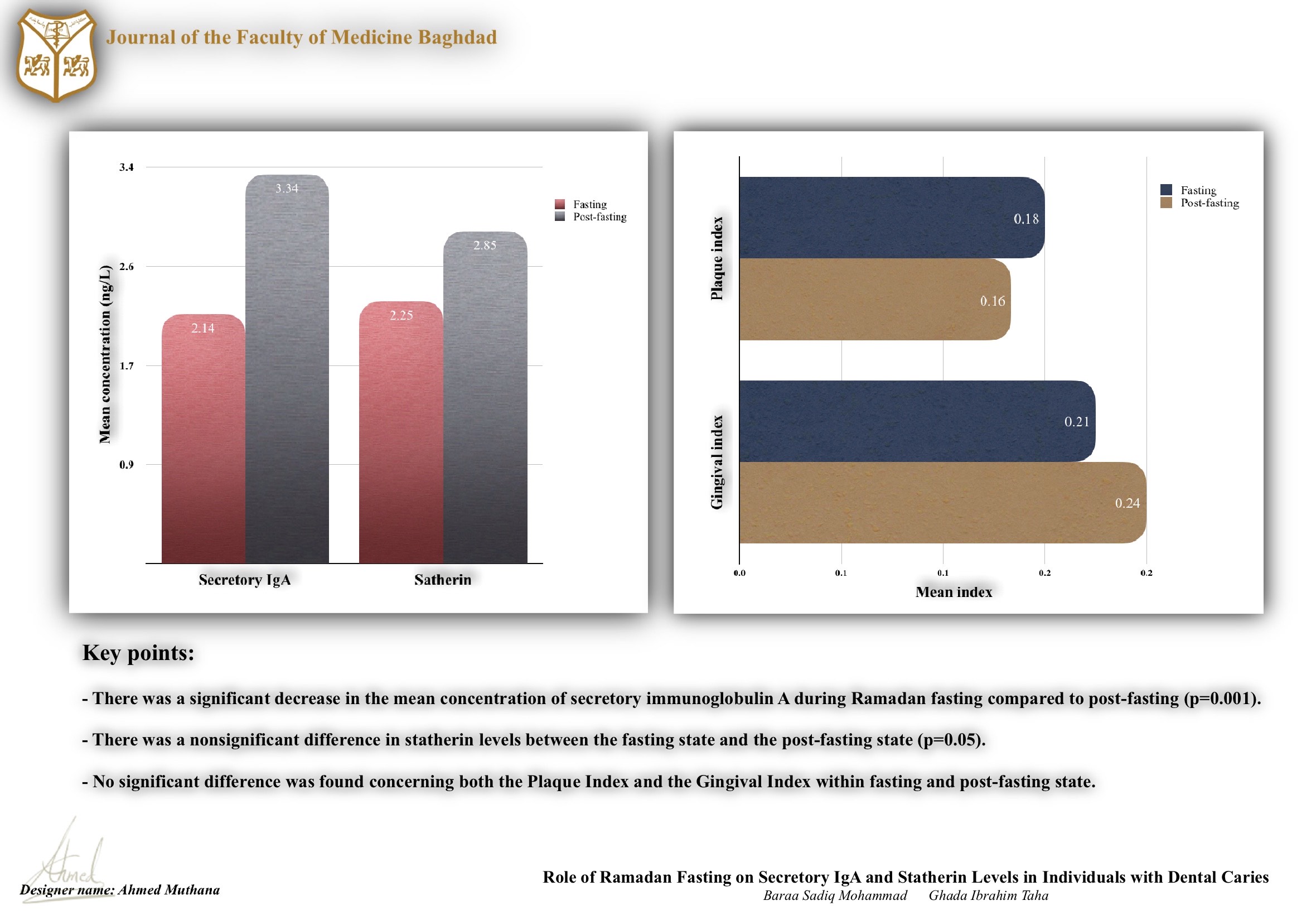
Results: A significant decrease in the mean concentration of secretory immunoglobulin A was observed during Ramadan fasting (2.14±0.21 ng/L) compared to post-fasting (3.34±0.35 ng/L) (p=0.001). However, there was a non-significant difference (p=0.05) in statherin levels between the fasting state (2.25±0.18 ng/L) and the post-fasting state (2.85±0.22 ng/L). No statistically significant difference was found concerning both the Plaque Index and the Gingival Index within fasting and post-fasting state.
Conclusion: Low concentration of sIgA and Statherin during Ramadan fasting may indicate altered salivary gland activity or systemic response to fasting, potentially affecting oral health.
التنزيلات
المراجع
Joachim MV, Ghantous Y, Zaaroura S, Alkeesh K, Zoabi T, Abu El-Na'aj I. Does fasting during Ramadan increase the risk of the development of sialadenitis? BMC Oral Health. 2020; 20(1):156. http://dx.doi.org/10.1186/s12903-020-01139-x
Mohammadzadeh A, Roshanravan N, Mesri Alamdari N, Safaiyan A, Mosharkesh E, Hadi A, Barati M, Ostadrahimi A. The interplay between fasting, gut microbiota, and lipid profile. Int J Clin Pract. 2021; 75(10):e14591. http://dx.doi.org/10.1111/ijcp.14591.
Al Agili DE. A systematic review of population-based dental caries studies among children in Saudi Arabia. The Saudi Dental Journal. 2013; (1):3–11. Available from: http://dx.doi.org/10.1016/j.sdentj.2012.10.002
Bilbilova ZE. Dietary Factors, Salivary Parameters, and Dental Caries. Dental Caries. 2021; http://dx.doi.org/10.5772/intechopen.92392
Al-Ansari AA. Prevalence, severity and secular trends of dental caries among various Saudi populations: A literature review. Saudi Journal of Medicine and Medical Sciences 2014, 2(3), 142. http://dx.doi.org/10.4103/1658-631X.142496
Piekoszewska-Ziętek P, Turska-Szybka A, Olczak-Kowalczyk D. Salivary proteins and peptides in the aetiology of caries in children: Systematic literature review. Oral Dis. 2019;25(4):1048-1056. http://dx.doi.org/10.1111/odi.12953 .
Buzalaf MAR, Ortiz AC, Carvalho TS, Fideles SOM, Araújo TT, Moraes SM, Buzalaf NR, Reis FN. Saliva as a diagnostic tool for dental caries, periodontal disease and cancer: is there a need for more biomarkers? Expert Rev Mol Diagn. 2020;20(5):543-555. http://dx.doi.org/10.1080/14737159.2020.1743686
Al-Saeed AFH, Mohammed AT. Oral Health Status in Relation to Selected Salivary Elements among a Group of Gasoline Stations Workers. JBCD. 2013; 25(3):125–9. http://dx.doi.org/10.12816/0015009
Ali D, Taha G. Effect of Covid-19 vaccine on some immunological salivary biomarkers (sIgA and Interleukine-17): Received: Dec. 2022 Accepted: May, 2023. JFacMedBagdad. 2023; 65(2). https://doi.org/10.32007/jfacmedbagdad.2039
Asal HA, Diajil AR, Al-Asady F. Salivary Interleukin-6 Level in Iraqi Patients with Oral Lichen Planus receiving Platelet-Rich Plasma Injections. AL-Kindy College Medical Journal. 2023;19(2):44–9. http://dx.doi.org/10.47723/kcmj.v19i2.934
Taha SSh. Assessment of Salivary Secretory Immunoglobulin a ( sIg A ) Level during Fixed Orthodontic Treatment. JBCD. 2016;28(3):155–60. Available from: http://dx.doi.org/10.12816/0031123
Ahmad P, Hussain A, Carrasco-Labra A, Siqueira WL. Salivary Proteins as Dental Caries Biomarkers: A Systematic Review. Caries Res. 2022;56(4):385-398. https://doi.org/10.1159/000526942.
Fang Y, Qian J, Xu L, Wei W, Bu W, Zhang S, Lv Y, Li L, Zhao C, Gao X, Gu Y, Wang L, Chen Z, Wang X, Zhang R, Xu Y, Yang Y, Lu J, Yan Z, Wang M, Tang L, Yuan N, Wang J. Short-term intensive fasting enhances the immune function of red blood cells in humans. Immun Ageing. 2023;20(1):44. https://doi.org/10.1186/s12979-023-00359-3
Wilhelm C, Surendar J, Karagiannis F. Enemy or ally? Fasting as an essential regulator of immune responses. Trends Immunol. 2021;42(5):389-400. https://doi.org/10.1016/j.it.2021.03.007
Husham S, Taha G. Changes in levels of Interleukin-6 (IL-6) and Interleukin-8 (IL-8) in the Serum of Preterm Delivery Pregnant Women Affected by Gingivitis. J Fac Med Bagdad. 2023; 65 (4). https://doi.org/10.32007/jfacmedbagdad.2152
Jasim SS, Taha GI. Comparison between HSV-1 Ag detection techniques by ELISA and real-time PCR in breast cancer patients suffering from periodontitis. J Fac Med Bagdad. 2023; 65(3):227-33. https://doi.org/10.32007/jfacmedbagdad.2105
McGregor AJ, Hasnain M, Sandberg K, Morrison MF, Berlin M, Trott J. How to study the impact of sex and gender in medical research: a review of resources. Biol Sex Differ. 2016;7(Suppl 1):46. http://dx.doi.org/10.1186/s13293-016-0099-1
Tsukinoki K, Yamamoto T, Handa K, Iwamiya M, Saruta J, Ino S, Sakurai T. Detection of cross-reactive immunoglobulin A against the severe acute respiratory syndrome-coronavirus-2 spike 1 subunit in saliva. PLoS One. 2021;16(11):e0249979. http://dx.doi.org/10.1371/journal.pone.0249979
Okunseri C, Okunseri E, Garcia RI, Visotcky A, Szabo A. Predictors of dental care use: findings from the national longitudinal study of adolescent health. J Adolesc Health. 2013; 53(5):663-70. http://dx.doi.org/10.1016/j.jadohealth.2013.05.013
Silk H, Kwok A. Addressing Adolescent Oral Health: A Review. Pediatr Rev. 2017;38(2):61-68. http://dx.doi.org/10.1542/pir.2016-0134
Greenstein G, Polson A. The role of local drug delivery in the management of periodontal diseases: a comprehensive review. J Periodontol. 1998;69(5):507-20. http://dx.doi.org/10.1902/jop.1998.69.5.507
Peedikayil FC, Narasimhan D. Oral Health of Fasting Muslims. JNutr, F& H 2019, 7(2), 97-102. http://dx.doi.org/10.22038/JNFH.2019.39195.1185
Telgi RL, Tandon V, Tangade PS, Tirth A, Kumar S, Yadav V. Efficacy of nonsurgical periodontal therapy on glycaemic control in type II diabetic patients: a randomized controlled clinical trial. J Periodontal Implant Sci. 2013;43(4):177-82. http://dx.doi.org/10.5051/jpis.2013.43.4.177
Aripin NFK, Zahid NI, Rahim MAA, Yaacob H, Haris PI, Rahim ZHA, Hashim RA. review of salivary composition changes induced by fasting and its impact on health. Food Science and Human Wellness 2023, 13(1), 50-64. https://doi.org/10.26599/FSHW.2022.9250004
Li M, Wang Y, Sun Y, Cui H, Zhu SJ, Qiu HJ. Mucosal vaccines: Strategies and challenges. Immunology Letters [Internet]. 2020 Jan;217:116–25. Available from: http://dx.doi.org/10.1016/j.imlet.2019.10.013
Cermakian N, Lange T, Golombek D, Sarkar D, Nakao A, Shibata S, Mazzoccoli G. Crosstalk between the circadian clock circuitry and the immune system. Chronobiol Int. 2013; 30 (7): 870-88. http://dx.doi.org/10.3109/07420528.2013.782315 .
Nagai M, Noguchi R, Takahashi D, Morikawa T, Koshida K, Komiyama S, Ishihara N, Yamada T, Kawamura YI, Muroi K, Hattori K, Kobayashi N, Fujimura Y, Hirota M, Matsumoto R, Aoki R, Tamura-Nakano M, Sugiyama M, Katakai T, Sato S, Takubo K, Dohi T, Hase K. Fasting-Refeeding Impacts Immune Cell Dynamics and Mucosal Immune Responses. Cell. 2019; 178(5):1072-1087.e14. http://dx.doi.org/10.1016/j.cell.2019.07.047.
Pietrzak B, Tomela K, Olejnik-Schmidt A, Mackiewicz A, Schmidt M. Secretory IgA in Intestinal Mucosal Secretions as an Adaptive Barrier against Microbial Cells. Int J M Sci. 2020; 21(23):9254. http://dx.doi.org/10.3390/ijms21239254
Hay DI, Moreno EC. Statherin and the Acidic Proline-Rich Proteins. Human Saliva: Clinical Chemistry and Microbiology. 2021;131–50. http://dx.doi.org/10.1201/9781003210399-5
Li J, Li Y, Zhou Y, Wang C, Wu B, Wan J. Actinomycesand Alimentary Tract Diseases: A Review of Its Biological Functions and Pathology. BioMed Res Int. 2018; 1–8.: http://dx.doi.org/10.1155/2018/3820215
Marques RCR, da Silva JR, Vieira Lima CP, Stefani CM, Damé-Teixeira N. Salivary parameters of adults with diabetes mellitus: a systematic review and meta-analysis. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2022; 134(2):176–89. http://dx.doi.org/10.1016/j.oooo.2022.03.001
Chennaoui M, Desgorces F, Drogou C, Boudjemaa B, Tomaszewski A, Depiesse F, Burnat P, Chalabi H, Gomez-Merino D. Effects of Ramadan fasting on physical performance and metabolic, hormonal, and inflammatory parameters in middle-distance runners. Appl Physiol Nutr Metab. 2009; 34(4):587-94. http://dx.doi.org/10.1139/H09-014
Besbes A, Khemiss M, Bragazzi N, Ben Saad H. The Impacts of Ramadan Intermittent Fasting on Saliva Flow-Rate and Metabolic Data: A Systematic Review. Front Nutr. 2022, 6; 9: 873502. http://dx.doi.org/10.3389/fnut.2022.873502
التنزيلات
منشور
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Baraa S. Mohammad, Ghada I. Taha

هذا العمل مرخص بموجب Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


