Assessment of Malondialdehyde as a Biomarker of Oxidative Stress and Its Correlation with 25-hydroxy Vitamin D3 in Women with Polycystic Ovary Syndromeoxy Vitamin D3
DOI:
https://doi.org/10.32007/jfacmedbaghdad3141Keywords:
Body Mass Index, Malondialdehyde, Oxidative Stress, Polycystic Ovary Syndrome, Vitamin D3 DeficiencyAbstract
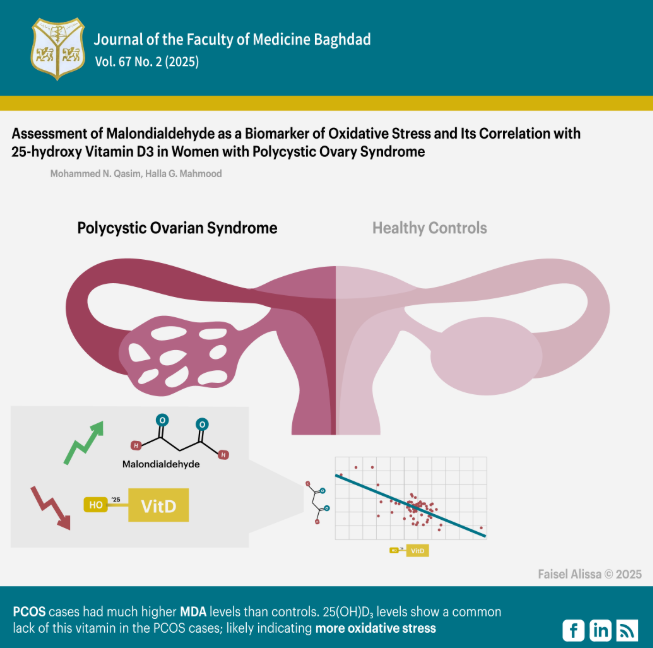
Background: Polycystic Ovary Syndrome (PCOS) is a prevalent endocrinology disorder affecting women in the years of reproduction. Malondialdehyde (MDA) is a result of polyunsaturated fatty acid peroxidation and is widely utilized as a trustworthy indicator of peroxidation of lipids and oxidative damage. Conversely, Vitamin D deficiency is a global issue affecting around one billion individuals. 25-hydroxyvitamin D₃ is linked to multiple metabolic processes and reproduction facets of women with PCOS and thus may contribute to the PCOS pathophysiology.
Objectives: To measure and compare serum malondialdehyde levels and 25-hydroxyvitamin D₃ concentrations between women with polycystic ovary syndrome (PCOS) versus age-matched healthy controls and to investigate the correlation between malondialdehyde and 25-hydroxyvitamin D₃ levels in both groups to elucidate potential mechanistic links between oxidative stress and vitamin D deficiency in PCOS pathophysiology.
Methods: The present case-control research was conducted at the Infertility Centre of Al-Batool Teaching Hospital, Diyala Governorate, Iraq, in collaboration with the Biochemistry Department at the College of Medicine, University of Baghdad, from April 2024 to January 2025. A total of 132 women aged 18-40 years were included in this study, comprising 66 PCOS cases and 66 healthy controls. A competitive enzyme-linked immunosorbent assay assessed the concentrations of serum malondialdehyde and 25-hydroxy vitamin D3.
Results: The results indicated markedly elevated serum malondialdehyde concentrations within the PCOS group compared to the controls. The concentrations of 25-hydroxy vitamin D3 in the PCOS group were considerably reduced compared to the controls. A significant negative correlation was found between serum malondialdehyde levels and 25-hydroxy vitamin D3 in the PCOS Group.
Conclusion: The current study showed that PCOS cases had much higher MDA levels than controls, probably indicating that they have experienced more oxidative stress. The level of 25(OH)D showed a common lack of this vitamin in the PCOS cases.
Received: April 2025
Revised: June 2025
Accepted: June 2025
Published Online: June 2025
Published: Oct. 2025
References
1. Mutashar M, Rasheed MK, Al-Naddawi AM. Association of Neuregulin-4 levels and body mass index with hyperandrogenism in Polycystic Ovary Syndrome patients. J Fac Med Baghdad. 2023;65(4).7. https://doi.org/10.32007/jfacmedbagdad.2140. DOI: https://doi.org/10.32007/jfacmedbagdad.2140
2. Abdelhamed MH, Al-Ghamdi WM, Al-Agha AE, Abdelhamed M, Al-Agha A. Polycystic ovary syndrome among female adolescents with congenital adrenal hyperplasia. Cureus. 2021;13(12).9. https://doi.org/10.7759/cureus.20698. DOI: https://doi.org/10.7759/cureus.20698
3. Rudnicka E, Duszewska AM, Kucharski M, Tyczyński P, Smolarczyk R. Oxidative Stress and Reproductive Function: Oxidative stress in polycystic ovary syndrome. Reproduction. 2022;164(6).10. https://doi.org/10.1530/REP-22-0152. DOI: https://doi.org/10.1530/REP-22-0152
4. Bai H, Ding H, Wang M. Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment. Clin Exp Obstet Gynecol. 2024;51(5).12. https://doi.org/10.31083/j.ceog5105126. DOI: https://doi.org/10.31083/j.ceog5105126
5. Zeidan K, Hassoon SM, Ahmed S. Polycystic ovary syndrome risk factors among women in baghdad: a case-control study. Health Educ Health Promot. 2022;10(3).5. http://hehp.modares.ac.ir/article-5-62991-en.html.
6. Soni T, Prabhakar PK. Pathophysiology of Polycystic Ovarian Syndrome. In: Polycystic Ovary Syndrome-Functional Investigation and Clinical Application. IntechOpen; 2022. https://doi.10.5772/intechopen.101921.
7. Qasim MN, Kadhem HK, El-Yassin HD. Correlation between vitamin D3 deficiency and serum leptin levels in a patient with polycystic ovary syndrome. Biochem Cell Arch. 2022;22(2).6. https://doi.org/10.51470/bca.2022.22.2.3773. DOI: https://doi.org/10.51470/bca.2022.22.2.3773
8. Vulcan T, Suciu TS, Lenghel LM, Toma VA, Decea N, Moldovan R, et al. The impact of vitamin D3 administration and of high fat diet on oxidative stress and inflammation in experimentally induced polycystic ovary syndrome. Med Pharm Reports. 2024;97(4).12. https://doi.org/10.15386/mpr-2798. DOI: https://doi.org/10.15386/mpr-2798
9. Hsieh CT, Yen TL, Chen YH, Jan JS, Teng RD, Yang CH, et al. Aging-Associated Thyroid Dysfunction Contributes to Oxidative Stress and Worsened Functional Outcomes Following Traumatic Brain Injury. Antioxidants. 2023;12(2).26. https://doi.org/10.3390/antiox12020217. DOI: https://doi.org/10.3390/antiox12020217
10. Aziz ASA, Elyaseen HD, Kadhem HK. Correlation between MDA Level and Chitotriosidase-1 Activity in Seminal Fluid of Iraqi Infertile Males. J Fac Med Baghdad. 2024;66(4).8. https://doi.org/10.32007/jfacmedbaghdad.6642395. DOI: https://doi.org/10.32007/jfacmedbaghdad.6642395
11. Chinko BC, Umeh OU. Alterations in lipid profile and oxidative stress markers following heat stress on wistar rats: Ameliorating role of vitamin C. Biomed Sci. 2023;9(1).6. https://doi.org/10.11648/j.bs.20230901.13. DOI: https://doi.org/10.11648/j.bs.20230901.13
12. Enechukwu CI, Onuegbu AJ, Olisekodiaka MJ, Eleje GU, Ikechebelu JI, Ugboaja JO, et al. Oxidative stress markers and lipid profiles of patients with polycystic ovary syndrome in a Nigerian tertiary hospital. Obstet Gynecol Sci. 2019;62(5).9.
https://doi.org/10.5468/ogs.2019.62.5.335. DOI: https://doi.org/10.5468/ogs.2019.62.5.335
13. Reczkowicz J, Mika A, Antosiewicz J, Kortas J, Proczko-Stepaniak M, Śledziński T, et al. Bariatric Surgery Induced Changes in Blood Cholesterol Are Modulated by Vitamin D Status. Nutrients. 2022;14(10).8. https://doi.org/10.3390/nu14102000. DOI: https://doi.org/10.3390/nu14102000
14. Fichera M, Török P, Tesarik J, Corte LD, Rizzo G, Garzon S, et al. Vitamin D, reproductive disorders and assisted reproduction: evidences and perspectives. Int J Food Sci Nutr. 2020;71(3).10. https://doi.org/10.1080/09637486.2019.1661978. DOI: https://doi.org/10.1080/09637486.2019.1661978
15. Ihim AC, Onyenekwe CC, Eze NN, Obi PC, Osakue N, Awalu JC, et al. Evaluation of Some Hormones Total Antioxidant Capacity and Malondialdehyde Levels in Polycystic Ovarian Syndrome Women attending the gynaecology Clinic at Nnewi. J Drug Deliv Ther. 2024;14(5).5 https://doi.org/10.22270/jddt.v14i5.6539. DOI: https://doi.org/10.22270/jddt.v14i5.6539
16. Alaee S, Ekramzadeh M, Samare-Najaf M, Jahromi BN, Shokri S, Ghomashi F, et al. Nutritional Intake and Lifestyle in Infertile Women with and without Polycystic Ovary Syndrome: A Case-control Study. J Infertil Reprod Biol. 2024;12(4).16.
https://doi.org/10.18502/jirb.v12i4.17975. DOI: https://doi.org/10.18502/jirb.v12i4.17975
17. Murri M, Luque-Ramírez M, Insenser M, Ojeda-Ojeda M, Escobar-Morreale HF. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): a systematic review and meta-analysis. Hum Reprod Update. 2013;19(3).21. https://doi.org/10.1093/humupd/dms059. DOI: https://doi.org/10.1093/humupd/dms059
18. Ali SA, Mansour NA, Oudah RG. Correlation between Serum Uric Acid, Vitamin D and HbA1c in Polycystic Ovary Syndrome. J Obstet Gynecol. 2024;4(3).7. https://medicalresearch.be/index.php/jog/article/view/76.
19. Chełchowska M, Jurczewska J, Gajewska J, Mazur J, Szostak-W˛egierek D, Rudnicka E, et al. Antioxidant defense expressed as glutathione status and Keap1-Nrf2 system action in relation to anthropometric parameters and body composition in young women with polycystic ovary syndrome. Antioxidants. 2023;12(3).14. https://doi.org/10.3390/antiox12030730. DOI: https://doi.org/10.3390/antiox12030730
20. Morgante G, Darino I, Spanò A, Luisi S, Luddi A, Piomboni P, et al. PCOS physiopathology and vitamin D deficiency: biological insights and perspectives for treatment. J Clin Med. 2022;11(15).14. https://doi.org/10.3390/jcm11154509. DOI: https://doi.org/10.3390/jcm11154509
21. Abow FH, Alsarraf ZH, Ali HJ. The role of vitamin D deficiency in Pathogenesis of PCOS: A case-control study among females in Mosul city. Iraqi J Med Sci. 2024; 22 (2).13. https://doi.10.22578/IJMS.22.2.8.
22. Hussein K. Association of vitamin D deficiency with metabolic factors in a cohort of Saudi women with polycystic ovary syndrome. Res Sq. 2022. https://doi.org/10.21203/rs.3.rs-2073766/v1. DOI: https://doi.org/10.21203/rs.3.rs-2073766/v1
23. Nowak A, Wojtowicz M, Baranski K, Galczynska D, Daniluk J, Pluta D. The correlation of vitamin D level with body mass index in women with polycystic ovary syndrome. Ginekol Pol. 2023;94(11).6. https://doi.org/10.5603/GP.a2023.0037. DOI: https://doi.org/10.5603/GP.a2023.0037
24. Babhulkar P, Tiwaskar S, Pathade A. Deficiency of vitamin D in India. J Pharm Negat Results. 2022;13(8).12.
https://doi.org/10.47750/pnr.2022.13.S08.19.
25. Klisic A, Malenica M, Kostadinovic J, Kocic G, Ninic A. Malondialdehyde as an independent predictor of body mass index in adolescent girls. J Med Biochem. 2023;42(2).8. https://doi.org/10.5937/jomb0-39044. DOI: https://doi.org/10.5937/jomb0-39044
26. Uçkan K, Demir H, Turan K, Sarıkaya E, Demir C. Role of oxidative stress in obese and nonobese PCOS patients. Int J Clin Pract. 2022;2022(2).9. https://doi.org/10.1155/2022/4579831. DOI: https://doi.org/10.1155/2022/4579831
27. Siahaan SC, Idarto A, Lestari SH, Usman F, Tannus FA. Correlation of Vitamin D Levels with Insulin Resistance in women with PCOS. Res J Pharm Technol. 2023;16(12).5. http://dx.doi.org/10.52711/0974-360X.2023.00948. DOI: https://doi.org/10.52711/0974-360X.2023.00948
28. Alawad ZM. Level of follicular fluid vitamin D and embryo quality in a sample of Iraqi women undergoing IVF. J Fac Med Baghdad. 2018;60(4).7. https://doi.org/10.32007/jfacmedbagdad.604758. DOI: https://doi.org/10.32007/jfacmedbagdad.604758
29. Shilpasree AS, Kulkarni VB, Shetty P, Bargale A, Goni M, Oli A, et al. Induction of endometrial HOXA 10 gene expression by vitamin D and its possible influence on reproductive outcome of PCOS patients undergoing ovulation induction procedure. Indian J Endocrinol Metab. 2022;26(3).7. https://doi.org/10.4103/ijem.ijem_90_22. DOI: https://doi.org/10.4103/ijem.ijem_90_22
30. Rahsepar M, Mahjoub S, Esmaelzadeh S, Kanafchian M, Ghasemi M. Evaluation of vitamin D status and its correlation with oxidative stress markers in women with polycystic ovary syndrome. Int J Reprod Biomed. 2017;15(6).6. https://doi.org/10.29252/ijrm.15.6.345. DOI: https://doi.org/10.29252/ijrm.15.6.345
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Mohammed N Qasim , Halla Ghazi Mahmood

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


