Interprofessional Collaboration among Health Care Team Members in Critical Care Units: Highlighting the Professional Qualities
DOI:
https://doi.org/10.32007/jfacmedbaghdad2420Keywords:
Critical Care Unit, Inter-professional Collaboration, Multidisciplinary Care Team, Partnership Practice, TeamworkAbstract
Background: Interprofessional collaboration (IPC) is the best way to provide high-quality and safe healthcare for the patient, reduce costs and length of hospital stay, as well as increase job satisfaction of the staff. However, many factors may hinder the achievement of interprofessional collaboration (IPC), and these need to be determined.
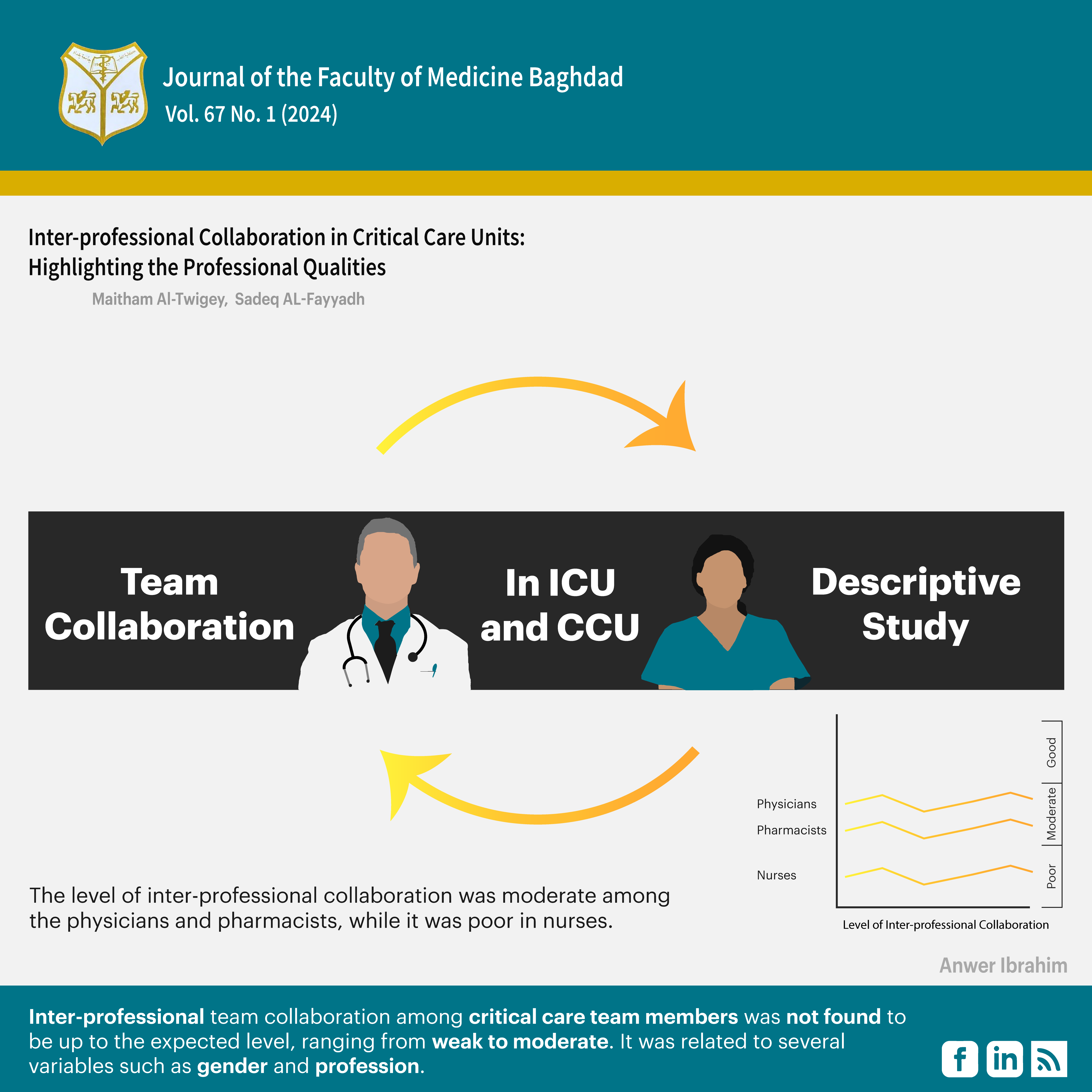
Objective(s): Determining the national status of interprofessional team collaboration among healthcare team members, including nurses, physicians, and clinical pharmacists, in Critical Care Units, and examining the statistical difference between the professional qualities of the subjects and their levels of interprofessional team collaboration, are the goals of this study.
Methods: A descriptive cross-sectional design was used in the present study. The current study was conducted in the Intensive Care Units (ICU) and Cardiac Care Units (CCU) of eight hospitals of the Najaf Governorate, in the Republic of Iraq. The 364 participants recruited in this study were healthcare team members, which included physicians, nurses, and pharmacists. The instrument used in the study is the Assessment of Interprofessional Team Collaboration Scale-II. Arithmetic means, frequencies, and percentages, as well as the Kruskal-Wallis and Mann-Whitney tests, were the statistical methods used in the study.
Results: The level of interprofessional collaboration (IPC) was moderate among the physicians with a mean score (MS) of 3.25, and pharmacists with 2.55, while it was lower in nurses at 2.06. Of equal importance, significant mean differences were observed between the overall scores of Interprofessional Team Collaboration among the healthcare team members and their sexes, number of physicians, academic preparation, specialization, work shift, and educational level.
Conclusion: The current study showed that Interprofessional Team Collaboration was not consistent with the standard expected level. Further, the professional qualities of many subjects exert significant effects on this level.
Received: Jul. 2024
Revised: Nov. 2024
Accepted: Dec. 2024
Published: April 2025
Downloads
References
1, Schilling S, Armaou M, Morrison Z, Carding P, Bricknell M, Connelly V. Understanding teamwork in rapidly deployed inter-professional teams in intensive and acute care: A systematic review of reviews. Plos one. 2022 Aug 18;17(8):e0272942. https://doi.org/10.1371/journal.pone.0272942
2. Bachynsky N. Implications for policy: The triple aim, quadruple aim, and inter-professional collaboration. InNursing forum 2020 Jan (Vol. 55, No. 1, pp. 54-64). https://doi.org/10.1371/journal.pone.0272942.
3. Moussa ML, Sofyani HA, Moussa FL, Alblowi BH, Oqdi YA, Khallaf S, et al. Effectiveness of Multidisciplinary Team Members in A Complex, High-Risk, And Stressful Critical Care Unit (CCU). Indonesian Journal for Health Sciences. 2020 Sep 1;4(2):99-107. https://doi.org/10.24269/ijhs.v4i2.2129.
4. Almutairi MS, Al Sulayyi NH, Alharbi AS, Alzarea NH, Sharif SA, Almosead MH, et al. The Importance Of Teamwork Between Operations And Anesthesia Technicians In The Operating Room. Journal of Namibian Studies: History Politics Culture. 2022 Oct 17;32:1093-104. https://doi.org/10.59670/xmtfph21.
5. Johnson JD. Network analysis approaches to collaborative information seeking in inter-professional health care teams. http://InformationR.net/ir/24-1/paper810.html.
6. Lai CC, Tseng KL, Ho CH, Chiang SR, Chen CM, Chan KS, et al. Prognosis of patients with acute respiratory failure and prolonged intensive care unit stay. Journal of thoracic disease. 2019 May;11(5):2051. https://doi.org/10.21037%2Fjtd.2019.04.84.
7. Scheuer CL, Voltan A, Kumanan K, Chakraborty S. Exploring the impact of decentralized leadership on knowledge sharing and work hindrance networks in healthcare teams. Journal of Management & Organization. 2023 Jan;29(1):139-58. https://doi.org/10.1017/jmo.2020.37.
8. Moreira FT, Callou RC, Albuquerque GA, Oliveira RM. Estratégias de comunicação efetiva no gerenciamento de comportamentos destrutivos e promoção da segurança do paciente. Revista Gaúcha de Enfermagem. 2019 Apr 29;40:e20180308. https://doi.org/10.1590/1983-1447.2019.20180308.
9. Donovan AL, Aldrich JM, Gross AK, Barchas DM, Thornton KC, Schell-Chaple HM, et al. Inter-professional care and teamwork in the ICU. Critical care medicine. 2018 Jun 1;46(6):980-90. https://doi.org/10.1097/CCM.0000000000003067.
10. Hennus MP, Young JQ, Hennessy M, Friedman KA, de Vries B, Hoff RG, et al. Supervision, inter-professional collaboration, and patient safety in intensive care units during the COVID-19 pandemic. ATS scholar. 2021 Sep;2(3):397-414. https://doi.org/10.34197/ats-scholar.2020-0165OC.
11. Michalsen A, Long AC, Ganz FD, White DB, Jensen HI, Metaxa V, et al. Inter-professional shared decision-making in the ICU: a systematic review and recommendations from an expert panel. Critical care medicine. 2019 Sep 1;47(9):1258-66. https://doi.org/10.1097/CCM.0000000000003870.
12. Kwan CW, Chan CW, Choi KC. The effectiveness of a nurse-led short term life review intervention in enhancing the spiritual and psychological well-being of people receiving palliative care: A mixed method study. International journal of nursing studies. 2019 Mar 1;91:134-43. https://doi.org/10.1016/j.ijnurstu.2018.12.007.
13. Shirey MR, Selleck CS, White-Williams C, Talley M, Harper DC. Inter-professional collaborative practice model to advance population health. Population Health Management. 2021 Feb 1;24(1):69-77. https://doi.org/10.1089/pop.2019.0194.
14. Yin J, Ma Z, Yu H, Jia M, Liao G. Transformational leadership and employee knowledge sharing: Explore the mediating roles of psychological safety and team efficacy. Journal of Knowledge Management. 2020 Mar 12;24(2):150-71. https://doi.org/10.1108/JKM-12-2018-0776.
15. Carney PA, Thayer EK, Palmer R, Galper AB, Zierler B, Eiff MP. The benefits of inter-professional learning and teamwork in primary care ambulatory training settings. Journal of inter-professional education & practice. 2019 Jun 1;15:119-26. https://doi.org/10.1016/j.xjep.2019.03.011.
16. Mahdizadeh M, Heydari A, Moonaghi HK. Exploration of the process of inter-professional collaboration among nurses and physicians in Iran. Electronic physician. 2017 Jun;9(6):4616. https://pubmed.ncbi.nlm.nih.gov/28848638.
17. Kaifi A, Tahir MA, Ibad A, Shahid J, Anwar M. Attitudes of nurses and physicians toward nurse–physician inter-professional collaboration in different hospitals of Islamabad–Rawalpindi Region of Pakistan. Journal of Inter-professional Care. 2021 Nov 2;35(6):863-8. https://doi.org/10.1080/13561820.2020.1853079.
18. Berry JC, Davis JT, Bartman T, Hafer CC, Lieb LM, Khan N, et al. Improved safety culture and teamwork climate are associated with decreases in patient harm and hospital mortality across a hospital system. Journal of patient safety. 2020 Jun 1;16(2):130-6. https://doi.org/10.1097/pts.0000000000000251.
19. Kang XL, Brom HM, Lasater KB, McHugh MD. The association of nurse–physician teamwork and mortality in surgical patients. Western journal of nursing research. 2020 Apr;42(4):245-53. https://doi.org/10.1177/0193945919856338.
20. Sorber R, Abularrage CJ. Diabetic foot ulcers: epidemiology and the role of multidisciplinary care teams. In: Seminars in vascular surgery 2021 Mar 1 (Vol. 34, No. 1, pp. 47-53). WB Saunders. https://doi.org/10.1053/j.semvascsurg.2021.02.006.
21. Walter C, Soni T, Gavin MA, Kubes J, Paciullo K. An inter-professional approach to reducing hospital-onset Clostridioides difficile infections. American Journal of Infection Control. 2022 Dec 1;50(12):1346-51. https://doi.org/10.1016/j.ajic.2022.02.017.
22. Sun R, Marshall DC, Sykes MC, Maruthappu M, Shalhoub J. The impact of improving teamwork on patient outcomes in surgery: A systematic review. International Journal of Surgery. 2018 May 1;53:171-7. https://doi.org/10.1016/j.ijsu.2018.03.044.
23. Mazer BL, Nabhan C. Strengthening the medical error “meme pool”. Journal of general internal medicine. 2019 Oct;34(10):2264-7. https://doi.org/10.1007/s11606-019-05156-7.
24. Herzberg S, Hansen M, Schoonover A, Skarica B, McNulty J, Harrod T, et al. Association between measured teamwork and medical errors: an observational study of prehospital care in the USA. BMJ open. 2019 Oct 1;9(10):e025314. https://doi.org/10.1136/bmjopen-2018-025314.
25. Al Khalfan AA, Al Ghamdi AA, De Simone S, Hadi YH. The impact of multidisciplinary team care on decreasing intensive care unit mortality. Saudi Critical Care Journal. 2021 Apr 1;5(2):13-8. https://doi.org/10.4103/sccj.sccj_34_20.
26. Na SJ, Chung CR, Choi HJ, Cho YH, Sung K, Yang JH, et al. The effect of multidisciplinary extracorporeal membrane oxygenation team on clinical outcomes in patients with severe acute respiratory failure. Annals of intensive care. 2018 Dec;8:1-0. https://doi.org/10.1186/s13613-018-0375-9.
27. Bilfinger TV, Albano D, Perwaiz M, Keresztes R, Nemesure B. Survival outcomes among lung cancer patients treated using a multidisciplinary team approach. Clinical lung cancer. 2018 Jul 1;19(4):346-51. https://doi.org/10.1016/j.cllc.2018.01.006.
28. Russell TA, Fritschel E, Do J, Donovan M, Keckeisen M, Agopian VG, et al. Minimizing central line–associated bloodstream infections in a high-acuity liver transplant intensive care unit. American journal of infection control. 2019 Mar 1;47(3):305-12. https://doi.org/10.1016/j.ajic.2018.08.006.
29. Berry JC, Davis JT, Bartman T, Hafer CC, Lieb LM, Khan N, et al. Improved Safety Culture and Teamwork Climate Are Associated With Decreases in Patient Harm and Hospital Mortality Across a Hospital System. Journal of patient safety. 2020 Jun;16(2):130-6. https://doi.org/10.1097/pts.0000000000000251.
20. Maier C, Thatcher JB, Grover V, Dwivedi YK. Cross-sectional research: A critical perspective, use cases, and recommendations for IS research. International Journal of Information Management. 2023 Jun 1;70:102625. https://doi.org/10.1016/j.ijinfomgt.2023.102625.
31. Orchard C, Pederson LL, Read E, Mahler C, Laschinger H. Assessment of Inter-professional Team Collaboration Scale (AITCS): further testing and instrument revision. Journal of Continuing Education in the Health Professions. 2018 Jan 1;38(1):11-8. https://doi.org/10.1097/ceh.0000000000000193.
32. Bode SF, Giesler M, Heinzmann A, Krüger M, Straub C. Self-perceived attitudes toward inter-professional collaboration and inter-professional education among different health care professionals in pediatrics. GMS journal for medical education. 2016;33(2). https://doi.org/10.3205/zma001016.
33. Mäki-Asiala M, Kaakinen P, Pölkki T. Inter-professional collaboration in the context of pain management in neonatal intensive care: a cross-sectional survey. Pain Management Nursing. 2022 Dec 1;23(6):759-66. https://doi.org/10.1016/j.pmn.2022.08.006.
34. Habre MA, Dolansky M, Lotas M, Allam S, Fitzpatrick J. Inter-professional collaboration among nurses and physicians in Lebanon. Journal of Inter-professional Education & Practice. 2023 Sep 1;32:100627. https://doi.org/10.1016/j.xjep.2023.100627.
35. Dulko D, Zangaro GA. Comparison of factors associated with physician and nurse burnout. Nursing Clinics. 2022 Mar 1;57(1):53-66. https://doi.org/10.1016/j.cnur.2021.11.004.
36. Flaherty E, Bartels SJ. Addressing the community‐based geriatric healthcare workforce shortage by leveraging the potential of inter-professional teams. Journal of the American Geriatrics Society. 2019 May;67(S2):S400-8. https://doi.org/10.1111/jgs.15924.
37. Ylitörmänen T, Kvist T, Turunen H. Perceptions on nurse–nurse collaboration among registered nurses in Finland and Norway. Scandinavian journal of caring sciences. 2019 Sep;33(3):731-40. https://doi.org/10.1111/scs.12669.
38. Degu T, Amsalu E, Kebede A, Adal O. Inter-professional collaboration and associated factors among nurses and physicians in specialized public hospitals, the northwest, Ethiopia: mixed method multi-centered cross-sectional study. BMC Health Services Research. 2023 Mar 27;23(1):286. https://doi.org/10.1186/s12913-023-09200-5.
39. Okab AA. Impact of Job Satisfaction on Job Performance of Nurses at Al-SuwairaGeneral Hospital. Iraqi National Journal of Nursing Specialties. 2017;30(2). https://doi.org/10.58897/injns.v30i2.282,
40. Jepkosgei J, English M, Adam MB, Nzinga J. Understanding intra-and inter-professional team and teamwork processes by exploring facility-based neonatal care in Kenyan hospitals. BMC Health Services Research. 2022 May 13;22(1):636. https://doi.org/10.1186/s12913-022-08039-6.
41. Hwang AY, Gums TH, Gums JG. The benefits of physician-pharmacist collaboration. The Journal of family practice. 2017 Dec 1;66(12):E1-8. https://pubmed.ncbi.nlm.nih.gov/29202145/.
42. Löffler C, Koudmani C, Böhmer F, Paschka SD, Höck J, Drewelow E, et al. Perceptions of inter-professional collaboration of general practitioners and community pharmacists-a qualitative study. BMC health services research. 2017 Dec;17:1-7. https://doi.org/10.1186/s12913-017-2157-8.
43. Albassam A, Almohammed H, Alhujaili M, Koshy S, Awad A. Perspectives of primary care physicians and pharmacists on inter-professional collaboration in Kuwait: A quantitative study. PloS one. 2020 Jul 20;15(7):e0236114. https://doi.org/10.1371/journal.pone.0236114.
44. Zielińska-Tomczak Ł, Cerbin-Koczorowska M, Przymuszała P, Gałązka N, Marciniak R. Pharmacists’ perspectives on inter-professional collaboration with physicians in Poland: A quantitative study. International Journal of Environmental Research and Public Health. 2021 Sep 14;18(18):9686. https://doi.org/10.3390/ijerph18189686.
45. Wrześniewska-Wal I, Pinkas J, Ostrowski J, Jankowski M. Pharmacists’ Perceptions of Physician–Pharmacist Collaboration—A 2022 Cross-Sectional Survey in Poland. In: Healthcare MDPI. 2023;11(17):2444). https://doi.org/10.3390/healthcare11172444.
46. Kucukarslan S, Lai S, Dong Y, Al-Bassam N, Kim K. Physician beliefs and attitudes toward collaboration with community pharmacists. Research in Social and Administrative Pharmacy. 2011 Sep 1;7(3):224-32. https://doi.org/10.1016/j.sapharm.2010.07.003.
47. Funk KA, Wahie N, Senne N, Funk RJ. Primary care provider demographics and engagement in inter-professional collaboration. The Journal of the American Board of Family Medicine. 2023 Feb 8;36(1):88-94. https://doi.org/10.3122/jabfm.2022.210463R1.
48. Helzer EG, Myers CG, Fahim C, Sutcliffe KM, Abernathy JH. Gender bias in collaborative medical decision making: emergent evidence. Academic Medicine. 2020 Oct 1;95(10):1524-8. https://doi.org/10.1097/acm.0000000000003590.
49. Ndibu Muntu Keba Kebe N, Chiocchio F, Bamvita JM, Fleury MJ. Variables associated with inter-professional collaboration: a comparison between primary healthcare and specialized mental health teams. BMC family practice. 2020 Dec; 21:1-1.https://doi.org/10.1186/s12875-019-1076-7.
50. Ross A, Bevans M, Brooks AT, Gibbons S, Wallen GR. Nurses and health-promoting behaviors: Knowledge may not translate into self-care. AORN journal. 2017 Mar 1;105(3):267-75. https://doi.org/10.1016/j.aorn.2016.12.018.
51. Lee KY, Zakaria N, Zakaria N. Examining the Impact of Burnout on Hospital Nurses Engaged in Shift Work: Insights From a Nationwide Cross-Sectional Study in Malaysia. SAGE Open Nursing. 2024 Apr;10:23779608241245212. https://doi.org/10.1177/23779608241245212.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Maitham A. Al-Twigey, Sadeq A. AL-Fayyadh

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


