Patients Preferences in Breaking Bad News: A Cross-Sectional Study
DOI:
https://doi.org/10.32007/jfacmedbaghdad2387Keywords:
Breaking Bad News, Cancer, Communication, Health care setting, SPIKESAbstract
Background: Doctors and patients communicating effectively is a very important base in cancer clinics and out-patient, the “Bad” news is any information that drastically alters a patient’s prospect of their life and forthcoming possibilities. It includes facts about diagnosis, recurrence, and treatment failure in clinical oncology settings.
Objective: To assess the attitudes of cancer patients toward receiving bad news of their condition and the relationships of some sociodemographic variables to these attitudes.
Methods: A cross-sectional study was conducted from the 19th of February to the 1st of June 2017 at the Oncology Hospital in the Medical City Teaching Centre/Baghdad. A group of 212 cases completed the questionnaire, which included socio-demographic information (age, gender, marital status, occupation, and education). The preference and attitude questions were set as in the recommended steps of the SPIKES protocol, which is a six-part method for sharing bad news with patients (Setting, Perception, Invitation, Knowledge, Emotions, and Summary).
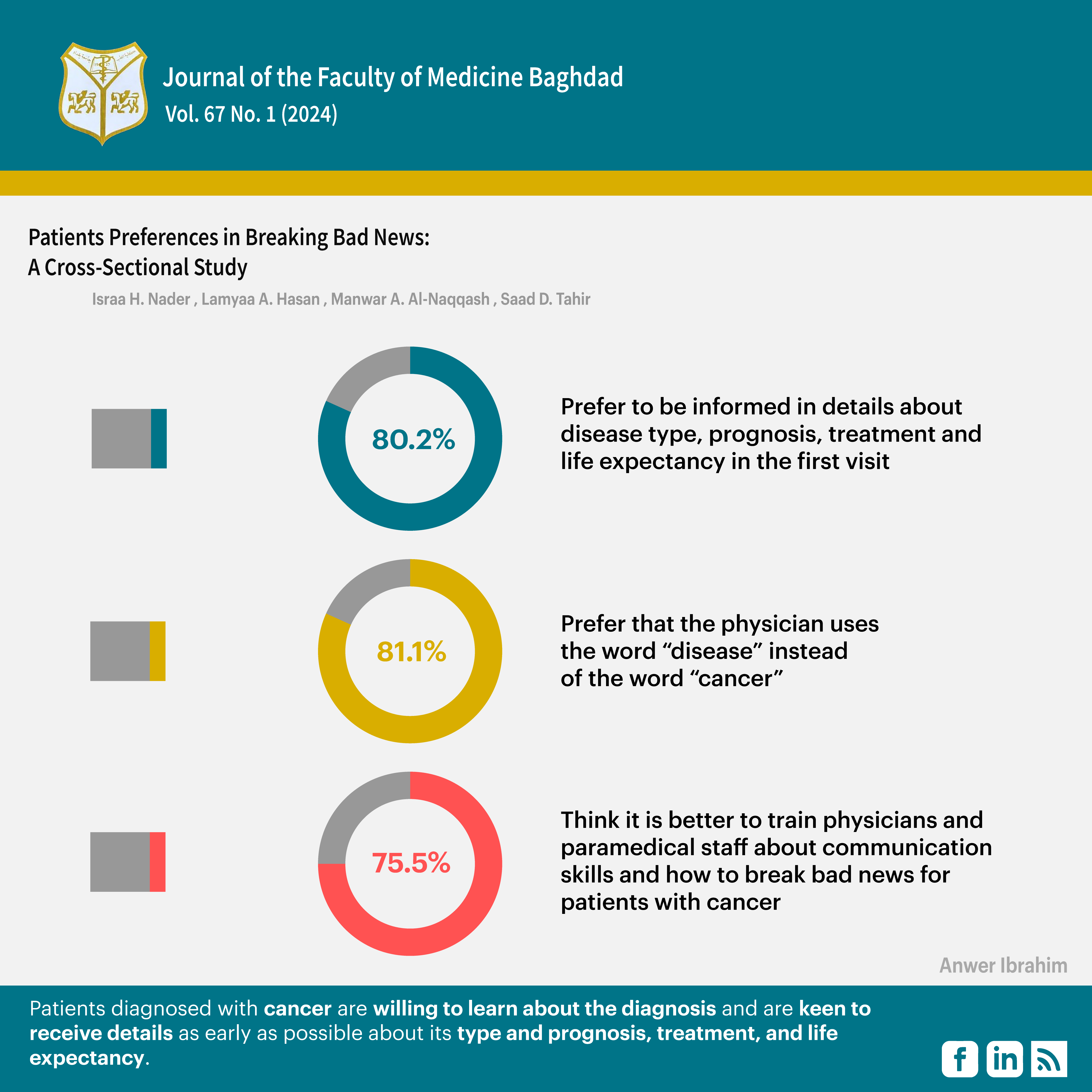
Result: Patients were classified into two age groups: those 50 years or older (64.2%) and those below 50 years (35.8%). Of the 212 cases, 46.2% were housewives, and 20.8% were government employees. The majority of patients (80.2%) preferred to be informed about their disease, its type, its prognosis, treatment, and life expectancy on the first visit. Most of the participants (67.9%) thought that the most experienced and skilled doctors have to notify them completely about their medical condition. The majority of them (81.1%) preferred that the physician use the word (disease) instead of "cancer. Most patients (75.5%) thought that it is better to train healthcare professionals in communication skills and how to break bad news.
Conclusion: Patients diagnosed with cancer are willing to learn about the diagnosis and are keen to receive details as early as possible about its type and prognosis, treatment, and life expectancy.
Received: Jul. 2024
Revised: Nov. 2024
Accepted: Jan. 2025
Published: April 2025
Downloads
References
1. Gill FJ, Hashem Z, Stegmann R, Aoun SM. The support needs of parent caregivers of children with a life-limiting illness and approaches used to meet their needs: a scoping review. Palliative Medicine. 2021;35(1):76-96. https://doi.org/10.1177/0269216320967593.
2. Pico M, Prado X, Guiñazú GG, Menéndez SD, Dvorkin J, López MV, et al. Communication of medical errors in a simulated clinical scenario. Experience with a pediatric residency group. Revista Paulista de Pediatria. 2023;42:e2022109. https://doi.org/10.1590/19840462/2024/42/2022109.
3. Kaye P. Breaking Bad News: a ten step approach. Scion Publishing Ltd; 2023
4. Krieger T, Salm S, Dresen A, Cecon N. Cancer patients’ experiences and preferences when receiving bad news: a qualitative study. Journal of cancer research and clinical oncology. 2023;149(7):3859-70. https://doi.org/10.1007/s00432-022-04311-8.
5. Wong HC, Wallen MP, Chan AW. Multinational Association of Supportive Care in Cancer (MASCC) clinical practice guidance for the prevention of breast cancer-related arm lymphoedema (BCRAL): international Delphi consensus-based recommendations. EClinicalMedicine. 2024;68. https://doi.org/10.1016/j.eclinm.2024.102441
6. Lundeby T, Finset A, Kaasa S. A complex communication skills training program for physicians providing advanced cancer care-content development and barriers and solutions for implementation. Journal of Communication in Healthcare. 2023; 16(1): 46-57. https://doi.org/10.1080/17538068.2022.2039468
7. Rubagumya F, Galica J, Rugengamanzi E, Niyibizi BA, Aggarwal A, Sullivan R, et al. Media coverage of cancer therapeutics: a review of literature. J Cancer Policy. 2023;36:100418. https://doi.org/10.1016/j.jcpo.2023.100418.
8. Smith MM, Secunda KE, Cohen ER, Wayne DB, Vermylen JH, Wood GJ. Clinical experience is not a proxy for competence: comparing fellow and medical student performance in a breaking bad news simulation-based mastery learning curriculum. American Journal of Hospice and Palliative Medicine®. 2023;40(4):423-30. https://doi.org/10.1177/10499091221106176.
9. Schmieder L, Gaynor K, Lynch J, D’Alton P. Perceived injustice and its impact on psychological distress in cancer patients and survivors. Supportive Care in Cancer. 2023;31(7):433.. https://doi.org/10.1007/s00520-023-07833-0
10. Porter AS, Chow E, Woods C, Lemmon ME, Baker JN, Mack JW, et al. Navigating prognostic communication when children with poor‐prognosis cancer experience prolonged disease stability. Pediatric Blood & Cancer. 2023;70(1):e29920.. https://doi.org/10.1002/pbc.29920.
11. Yoshida S, Shimizu K, Matsui M, Fujimori M, Uchitomi Y, Horibe K. Preferred communication with adolescent and young adult patients receiving bad news about cancer. J Adolesc Young Adult Oncol2023;12(4):561-8. https://doi.org/10.1089/jayao.2022.0073.
12. Jalali R, Jalali A, Jalilian M. Breaking bad news in medical services: a comprehensive systematic review. Heliyon. 2023; 9 (4). https://doi.org/10.1016/j.heliyon.2023.e14734
13. Martins BN, Migliorati CA, Ribeiro AC. The barriers dentists face to communicate cancer diagnosis: self-assessment based on SPIKES protocol. Medicina Oral, Patologia Oral y Cirugia Bucal. 2023;28(2):e191. https://doi.org/10.4317/medoral.25650.
14. Mahendiran M, Yeung H, Rossi S, Khosravani H, Perri GA. Evaluating the effectiveness of the SPIKES model to break bad news–a systematic review. Am J Hosp Palliat Care. 2023;40(11):1231-60. https://doi.org/10.1177/10499091221146296
15. Lounsbury DW, Nichols S, Asuzu C. Communicating bad news to patients and families in African oncology settings. Psycho‐Oncology. 2023;32(1):47-57. https://doi.org/10.1002/pon.6025.
16. von Blanckenburg P, Köhler C, Petzel A, Jülicher A, Schneider V, Schneider A. Quality of breaking bad news to patients diagnosed with neoplasia of the uterine cervix. Journal of Cancer Research and Clinical Oncology. 2023;149(19):17215-22. https://doi.org/10.1007/s00432-023-05442-2.
17. Akalu Y, Ayelign B, Molla M.D. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infection and drug resistance, 2020; 1949-1960. https://doi.org/10.2147/IDR.S258736.
18. Sabry SA, Ibrahem MJ, Jabarah MA. Relationship of the quality of life in capecitabine-treated colorectal cancer patients to sociodemographic characteristics and drug-related adverse effects. J Fac Med Baghdad. 2022;64(3):175-82. https://doi.org/10.32007/jfacmedbagdad.6431970.
19. Aminiahidashti H, Mousavi SJ, Darzi MM. Patients’ attitude toward breaking bad news; a brief report. Emergency. 2016; 4(1):34.
20. Alrukban MO, Albadr BO, Almansour M. Preferences and attitudes of the Saudi population toward receiving medical bad news: A primary study from Riyadh city. Journal of Family and Community Medicine. 2014;21(2):85-92.. https://doi.org/10.4103/2230-8229.134763
21. Karim SM, Baeshen W, Neamatullah SN, Bin B. Oral contraceptives, abortion and breast cancer risk: a case control study in Saudi Arabia. Asian Pacific Journal of Cancer Prevention. 2015;16(9):3957-60.https://doi.org/10.7314/APJCP.2015.16.9.3957.
22. Seifart C, Hofmann M, Bär T, Knorrenschild JR, Seifart U, Rief W. Breaking bad news–what patients want and what they get: evaluating the SPIKES protocol in Germany. Annals of Oncology. 2014;25(3):707-11. https://doi.org/10.1093/annonc/mdt582.
23. Koch M, and Seifart C. Rethinking parameters of "success" in breaking bad news conversations from patient's perspective: the successful delivery process model. Supportive Care in Cancer, 2024. 32(3): 181. https://doi.org/10.1007/s00520-024-08354-0.
24. Jenkins V, Catt S, Banerjee S, Gourley C, Montes A, Solis-Trapala I, et al. Patients’ and oncologists’ views on the treatment and care of advanced ovarian cancer in the UK: results from the ADVOCATE study. BJC. 2013;108(11):2264-71. https://doi.org/10.1038/bjc.2013.223.
25. Parker PA, Baile WF, de Moor C, Lenzi R, Kudelka AP, Cohen L. Breaking bad news about cancer: patients’ preferences for communication. JCO. 2001;19(7):2049-56. https://doi.org/10.1200/JCO.2001.19.7.2049.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Israa H. Nader, Lamyaa A. Hasan, Manwar A. Al-Naqqash, Saad D. Tahir

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


