Clinical and Cephalometric Assessments in Grade II and Grade IV Adenoid Hypertrophy: A Cross-Sectional Study
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632286Keywords:
Cephalometrics, Cross-sectional, Endoscopy, Grade II adenoid, Graded mirror , Hypertrophy, Lip-seal, Water-retentionAbstract
Background: Adenoid hypertrophy is one of the most common causes of nasal obstruction, and physicians use different methods to investigate it to reach a definite diagnosis.
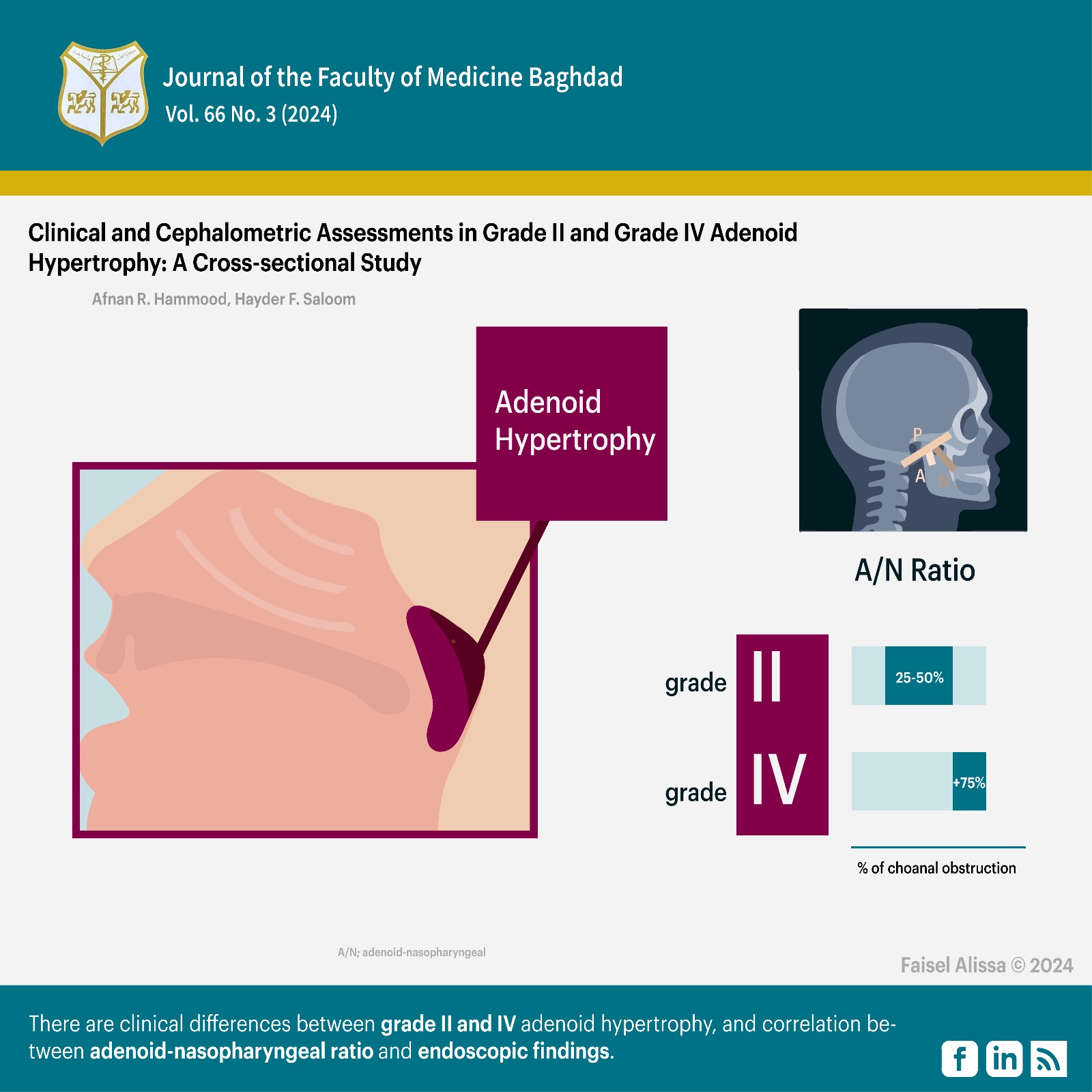
Objectives: This study aims to determine whether there are clinical differences between grade II and IV adenoid hypertrophy and whether there is a positive correlation between adenoid-nasopharyngeal ratio and endoscopic examination findings.
Methods: This study was carried out on 120 patients; they were confirmed with five clinical tests (graded mirror, water-retention, lip-seal, deep-breath, and functional tests) and lateral cephalometric radiographs to measure the adenoid-nasopharyngeal ratio. Kruskal-Wallis test was used for the mirror test, while the Chi-squared test was used for the rest to detect the differences among groups. Spearman's correlation coefficient test was used to determine the correlation between the adenoid-nasopharyngeal ratio and endoscopic findings.
Results: The age range of the patients was 6-12 years [mean age = 9.13 ± 1.97 years], 60.8% male, 39.2% female. Kruskal-Wallis and Chi-squared tests showed a statistically significant difference with P > 0.01 between groups. A strong positive significant correlation at P < 0.01, Spearman's test 0.94 was found between adenoid-nasopharyngeal ratio and endoscopic findings.
Conclusion: Lateral cephalogram and nasal endoscopy can detect most pathologies associated with airway blockage. There are clinical differences between grade II and grade IV adenoid hypertrophy, and there is a good correlation between the adenoid-nasopharyngeal ratio measured by lateral cephalogram and endoscopic findings.
Received: Dec. 2023
Revised: May 2024
Accepted: June,2024
Downloads
References
Niedzielski A, Chmielik LP, Mielnik-Niedzielska G, Kasprzyk A, Bogusławska J. Adenoid hypertrophy in children: a narrative review of pathogenesis and clinical relevance. BMJ Paediatrics Open. 2023; 7(1). https://doi.org/10.1136%2Fbmjpo-2022-001710.
Arambula A, Brown JR, Neff L. Anatomy and physiology of the palatine tonsils, adenoids, and lingual tonsils. World J Otorhinolaryngol Head Neck Surg. 2021; 7(03):155-160. https://pubmed.ncbi.nlm.nih.gov/34430822/.
Galić MZ, Klančnik M. Adenoid size in children with otitis media with effusion. Acta Clin Croat. 2021; 60(3):532-538. https://doi.org/10.20471%2Facc.2021.60.03.25.
Ohuche IO, Iloanusi NI, Dike CM, Chime EN. Clinical presentation, radiographic findings, and treatment outcomes in children with adenoid hypertrophy in a paediatric outpatient clinic in Enugu, Nigeria. Ghana Med J. 2023; 57(3). http://dx.doi.org/10.4314/gmj.v57i3.7.
Al-Sheakli II, Mohammed SA, Taha SS. The frontal sinus dimensions in mouth and nasal breathers in Iraqi adult subjects. J Bagh Coll Dent. 2013; 25(2):155-63. https://jbcd.uobaghdad.edu.iq/index.php/jbcd/article/view/245.
Zhao Z, Zheng L, Huang X, Li C, Liu J, Hu Y. Effects of mouth breathing on facial skeletal development in children: a systematic review and meta-analysis. BMC Oral Health. 2021; 21(article 108). https://link.springer.com/article/10.1186/s12903-021-01458-7.
Feng X, Chen Y, Cai W, Lie SA, Hellén-Halme K, Shi X-Q. Aerodynamic characteristics in upper airways among orthodontic patients and its association with adenoid nasopharyngeal ratios in lateral cephalograms. BMC Med Imaging. 2021; 21(article 127). https://doi.org/10.1186/s12880-021-00659-4.
Yoon A, Gozal D, Kushida C, Pelayo R, Liu S, Faldu J, et al. A roadmap of craniofacial growth modification for children with sleep-disordered breathing: a multidisciplinary proposal. Sleep. 2023; 46(8):zsad095. https://doi.org/10.1093/sleep/zsad095.
Zwierz A, Domagalski K, Masna K, Burduk P. Effectiveness of evaluation of adenoid hypertrophy in children by flexible nasopharyngoscopy examination (FNE), proposed schema of frequency of examination: Cohort study. Diagnostics. 2022; 12(7):1734 https://doi.org/10.3390/diagnostics12071734.
Pathak K, Ankale NR, Harugop AS. Comparison Between Radiological Versus Endoscopic Assessment of Adenoid Tissue in Patients of Chronic Adenoiditis. Indian J Otolaryngol Head Neck Surg. 2019; 71:981-985. https://doi.org/10.1007/s12070-019-01669-z.
Cassano M, De Corso E, Fiore V, Giancaspro R, Moffa A, Casale M, et al. Update of endoscopic classification system of adenoid hypertrophy based on clinical experience on 7621 children. Acta Otorhinolaryngol Ital. 2022; 42(3):257-264. https://pubmed.ncbi.nlm.nih.gov/35396589/.
Monteiro A, Koch HA, Linder-Aronson S. Evaluation of the Nasopharyngeal Free Airway Space based on Lateral Cephalometric Radiographs and Endoscopy. Orthodontics. 2004; 1(3). 1-9. URL
Pacheco MCT, Casagrande CF, Teixeira LP, Finck NS, Araújo MTMd. Guidelines proposal for clinical recognition of mouth breathing children. Dental press j orthod. 2015; 20(4). https://doi.org/10.1590/2176-9451.20.4.039-044.oar
Kadhom ZM, Jumaa N. Natural head position: A review. J Bagh Coll Dent. 2020; 32(3):19-22 DOI: https://doi.org/10.26477/jbcd.v32i3.2896.
Yassir YA, Nabbat SA, Hamdan HA. Evaluation of Semi-Automated Software and Application for Cephalometric Analysis. International Medical Journal. 2021; 28(1):16-20. URL
Fujioka M, Young LW, Girdany BR. Radiographic evaluation of adenoidal size in children: adenoidal-nasopharyngeal ratio. AJR Am j Roentgenol. 1979; 133(3):401-404. https://doi.org/10.2214/ajr.133.3.401.
Moideen SP, Mytheenkunju R, Govindan Nair A, Mogarnad M, Afroze MKH. Role of adenoid-nasopharyngeal ratio in assessing adenoid hypertrophy. Indian J Otolaryngol Head Neck Surg. 2019; 71:469-473. https://doi.org/10.1007%2Fs12070-018-1359-7.
Yassir YA, Salman AR, Nabbat SA. The accuracy and reliability of WebCeph for cephalometric analysis. J Taibah Univ Med Sci. 2022; 17(1):57-66. https://doi.org/10.1016/j.jtumed.2021.08.010.
Achmad H, Ansar AW. Mouth breathing in pediatric population: a literature review. Ann Rom Soc Cell Biol. 2021; 25(6):4431-4455. http://www.annalsofrscb.ro/index.php/journal/article/view/6275.
Lin L, Zhao T, Qin D, Hua F, He H. The impact of mouth breathing on dentofacial development: A concise review. Front Public Health. 2022; 10(article 929165). https://doi.org/10.3389/fpubh.2022.929165.
Cummings S, Chambers DW. Diagnostic paths for a mouth-breathing patient. Am J Orthod Dentofacial Orthop. 2020; 158(4):564-571. e2. https://pubmed.ncbi.nlm.nih.gov/32829973/.
Abdelghany AM, Elsamanody AN. A simple home test to differentiate habitual from pathological mouth breathing. Int J Pediatr Otorhinolaryngo. 2023; 174(article 111719). https://doi.org/10.1016/j.ijporl.2023.111719.
Morais-Almeida M, Wandalsen GF, Solé D. Growth and mouth breathers. Jornal de pediatria. 2019; 95:66-71. https://doi.org/10.1016/j.jped.2018.11.005.
Kalaskar R, Bhaje P, Kalaskar A, Faye A. Sleep Difficulties and Symptoms of Attention-deficit Hyperactivity Disorder in Children with Mouth Breathing. Int J Clin Pediatr Dent. 2021; 14(5):604-609. https://pubmed.ncbi.nlm.nih.gov/34934269/.
Zheng W, Zhang X, Dong J, He J. Facial morphological characteristics of mouth breathers vs. nasal breathers: A systematic review and meta‑analysis of lateral cephalometric data. Experimental and Therapeutic Medicine. 2020; 19(6):3738-3750. https://www.spandidos-publications.com/10.3892/etm.2020.8611.
Zwierz A, Masna K, Domagalski K, Burduk P. 150th Anniversary of global adenoid investigations: Unanswered questions and unsolved problems. Front Pediatr. 2023; 11(article 1179218). https://doi.org/10.3389%2Ffped.2023.1179218.
Saibene AM, Rosso C, Pipolo C, Lozza P, Scotti A, Ghelma F, et al. Endoscopic adenoidectomy: a systematic analysis of outcomes and complications in 1006 patients. Acta Otorhinolaryngol Ital. 2020; 40(1):79-86. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7147541/.
Calvo-Henriquez C, Branco AM, Lechien JR, Maria-Saibene A, DeMarchi MV, Valencia-Blanco B, et al. What is the relationship between the size of the adenoids and nasal obstruction? A systematic review. Int J Pediatr Otorhinolaryngol. 2021; 151(article 110895) https://doi.org/10.1016/j.ijporl.2021.110895.
Ishida T, Manabe A, Yang S-S, Yoon HS, Kanda E, Ono T. Patterns of adenoid and tonsil growth in Japanese children and adolescents: A longitudinal study. Sci Rep. 2018; 8(article17088). https://doi.org/10.1038/s41598-018-35272-z.
Modather M, Saad GM, Weshahy H, Ibrahim R, Osman ME. Assessment of Adenoid Size Using Flexible Nasoendoscopy and Lateral Neck Radiography and Its Relation to Clinical Symptoms. Egypt J Neck Surg Otorhinolaryngol. 2023; 9(3):13. https://doi.org/10.21608/ejnso.2023.231456.1083.
Zhao T, Zhou J, Yan J, Cao L, Cao Y, Hua F, et al. Automated adenoid hypertrophy assessment with lateral cephalometry in children based on artificial intelligence. Diagnostics. 2021; 11(8):1386 https://doi.org/10.3390/diagnostics11081386.
He Z, Xiao Y, Wu X, Liang Y, Zhou Y, An G. An Automatic Assessment Model of Adenoid Hypertrophy in MRI Images based on Deep Convolutional Neural Networks. IEEE Access. 2023; 11:106516 - 106527 https://doi.org/10.1109/ACCESS.2023.3316689
Tursun S, Muluk NB, Özdemir A, Özel G, Şencan Z. Maxillary sinus volume and adenoid tissue size in children: computed tomographic evaluation. Romanian Journal of Rhinology. 2023; 13(52):158-164. https://doi.org/10.2478/rjr-2023-0024.
Kalaskar R, Balasubramanian S, Kalaskar A. Evaluation of the Average Nasal and Nasopharyngeal Volume in 10–13-year-old Children: A Preliminary CBCT Study. Int J Clin Pediatr Dent. 2021; 14(2):187-191https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8343683/.
Al-Khawaja NFK, Nahidh M, Abdulsaheb RJ. Assessment of maxillary incisors' angulation and position in different types of malocclusions using cone-beam computed tomography. Contemp Clin Dent. 2021; 12(4):401-407 https://pubmed.ncbi.nlm.nih.gov/35068840/.
Talebian S, Sharifzadeh G, Vakili I, Golboie SH. Comparison of adenoid size in lateral radiographic, pathologic, and endoscopic measurements. Electronic physician. 2018; 10(6):6935–6941 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6049977/.
Major MP, Saltaji H, El-Hakim H, Witmans M, Major P, Flores-Mir C. The accuracy of diagnostic tests for adenoid hypertrophy: a systematic review. J Am Dent Assoc. 2014; 145(3):247-54. https://pubmed.ncbi.nlm.nih.gov/24583889/.
Schupper AJ, Nation J, Pransky S. Adenoidectomy in children: what is the evidence and what is its role? Curr Otorhinolaryngol Rep. 2018; 6:64-73. https://doi.org/10.1007/s40136-018-0190-8.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Afnan R. Razaq, Hayder F. Saloom

This work is licensed under a Creative Commons Attribution 4.0 International License.










 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


