Association between Alpha- Klotho Protein, Calcium, and Phosphate concentrations in Adult Iraqi Patients with Beta-Thalassemia Major
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6642391Keywords:
Calcium, Ferritin, Klotho, Phosphate, ThalassemiaAbstract
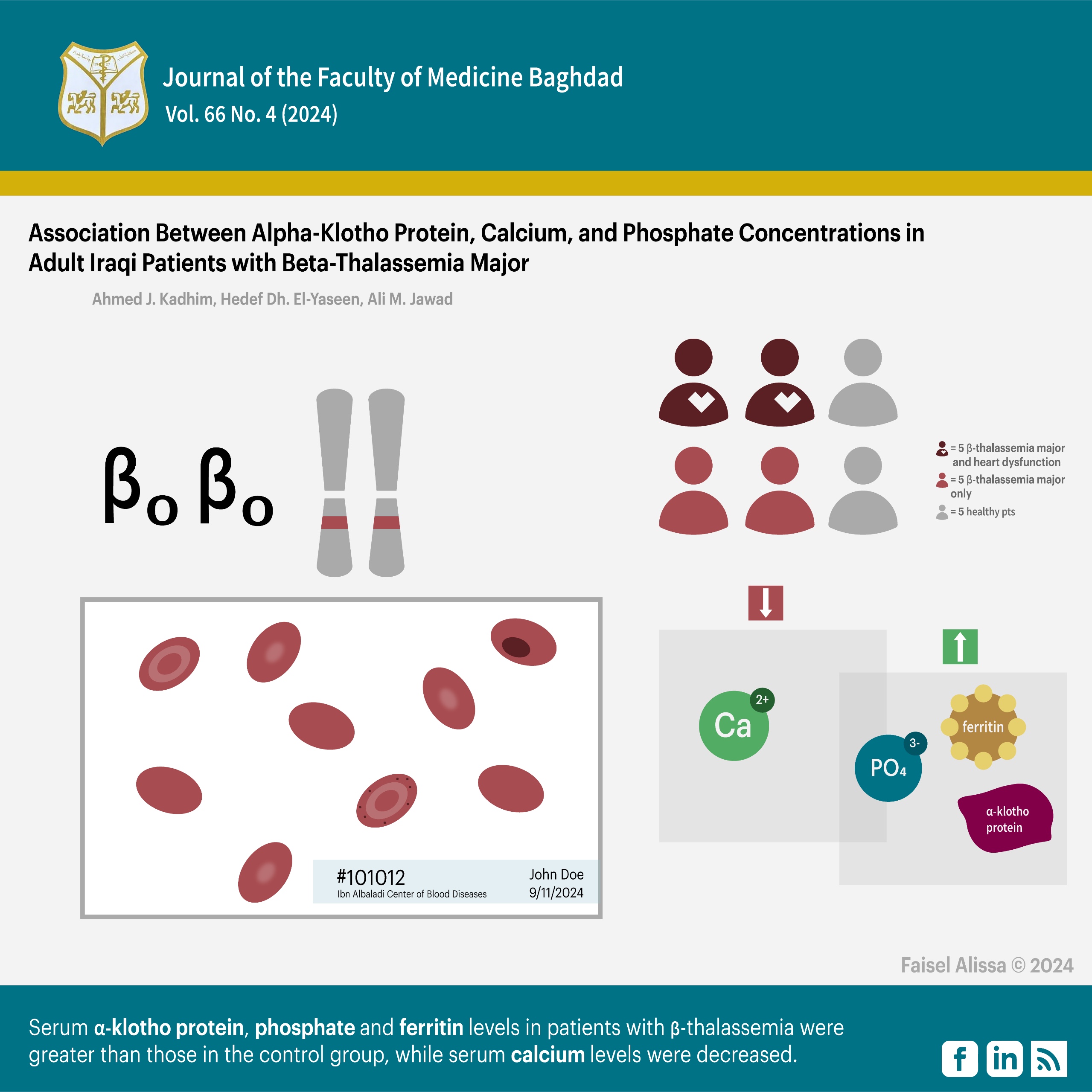
Background: Beta-thalassemia major is a prevalent global condition characterized by a rapid breakdown of red blood cells. Regular blood transfusions can give rise to problems such as cardiovascular disease, diabetes, osteoporosis, and renal disorders. Alpha-Klotho protein is a protein that has anti-aging properties and is involved in several functions, including reducing oxidative stress, regulating energy metabolism through several routes, and managing calcium and phosphate metabolism.
Objective: This study aimed to assess changes in calcium and phosphate levels, Alpha-Klotho protein concentration, and their associations with cardiac dysfunction in patients with Beta-thalassemia major.
Methods: The study was conducted at Al-Sadr General Hospital and Ibn Albaladi Center of Blood Diseases, Baghdad, and involved 90 participants who were grouped into three groups: Group A: 30 patients with Beta-thalassemia major and heart dysfunction; Group B:30 patients with Beta-thalassemia major without any signs of heart dysfunction; and Group C:30 healthy individuals as a control group. The indicators examined were serum levels of Alpha-klotho protein, calcium, phosphate, and Ferritin. ELISA method was used to assess serum Alpha-klotho protein, whereas serum Ca, serum phosphate, and serum Ferritin were analyzed using the Beckman Coulter AU clinical chemistry analyzers.
Results: The mean values of Serum Alpha-Klotho protein, phosphate, and Ferritin in the patients with beta-thalassemia were greater than those in the control group with P value<0.05. Patients with thalassemia had decreased levels of serum calcium compared to the control group. Additionally, a strong negative association was observed between serum calcium and phosphate levels.
Conclusion: Patients with beta-thalassemia major have significant alterations in calcium and phosphate levels under the control of Klotho protein levels.
Received: May 2024
Revised: Aug. 2024
Accepted: Sep. 2024
Published: Dec. 2024
Downloads
References
1. Zeiny SM. The correlation between HLA class II and β-thalassemia major in Al-Karama Teaching Hospital. J Fac Med Baghdad. 2016;58(4):366–70. https://doi.org/10.32007/jfacmedbagdad.584287.
2. Faraj SA. Hemostatic parameters in Thalassemia patients; a single institute experience. J Fac Med Baghdad. 2016; 58(2):132–5. https://doi.org/10.32007/jfacmedbagdad.582223.
3. Mohammad RL, Sadiq F, Hashem A. Information and practice of self-administration about the injection of Deferoxamine among adolescent thalassemia patients in the al-Najef city. Ann Rom Soc Cell Biol. 2021 May 20; 25(6): 2413–7. https://annalsofrscb.ro/index.php/journal/article/view/5856.
4. Liu Y, Yang R, Liu J, Meng D, Zhou Z, Zhang Y, et al. Fabrication, structure, and function evaluation of the ferritin-based nano-carrier for food bioactive compounds. Food Chem. 2019 Nov 30;299:125097. https://doi.org/10.1016/j.foodchem.2019.125097.
5. Soliman A, Yassin M, Alyafei F, Alaaraj N, Hamed N, Osman S, et al. Nutritional studies in patients with β-thalassemia major: A short review. Acta Biomed. 2023;94(3):1–14. https://doi.org/10.23750%2Fabm.v94i3.14732.
6. Sultana MA, Akhter QS. Serum calcium and serum phosphate levels in transfusion-dependent beta-thalassemia. J Bangladesh Soc Physiol. 2018 Dec 26;13(2):54–8. http://dx.doi.org/10.3329/jbsp.v13i2.39478.
7. Neyra JA, Hu MC, Moe OW. Klotho in Clinical Nephrology: Diagnostic and Therapeutic Implications. Clin J Am Soc Nephrol. 2021 Jan 1 ;16(1):162. https://doi.org/10.2215/cjn.02840320.
8. Portales-Castillo I, Simic P. PTH, FGF-23, Klotho and Vitamin D as regulators of calcium and phosphorus: Genetics, epigenetics and beyond. Front Endocrinol (Lausanne). 2022 Sep 29; 13:992666. https://doi.org/10.3389%2Ffendo.2022.992666.
9. Navarro-Garcia JA, Rueda A, Romero-Garcia T, Accedes-Ripoll J, Rodríguez-Sánchez E, González-LA Fuente L, et al. Enhanced Klotho availability protects against cardiac dysfunction induced by uremic cardiomyopathy by regulating Ca2+ handling. Br J Pharmacol. 2020;177(20):4701–19. https://doi.org/10.1111/bph.15235
10. Talib NH, Al-Yaseen HD, Jawad AM. Serum Preptin Level in Iraqi Beta Major Thalassemia Patients. Indian J Forensic Med Toxically. 2022;16(1):913–9. https://doi.org/10.37506/ijfmt.v16i1.17614.
11. Ali EA, Agbayani AA, Alabaman SA, Altham KA. Serum hepcidin and ferritin level changes in Iraqi adult patients with non-transfusion dependent beta-thalassemia major and intermedia. Int J Pharm Res. 2020;13(1):1373–8. https://doi.org/10.31838/ijpr/2021.13.01.301.
12. Maki Al-Hindy HAA, Mousa MJ, Shaker AK. No significant relationship of ferritin levels to the levels of platelet-derived growth factor (PDGF) in the peripheral blood of transfusion-dependent β-thalassemia major patients with growth retardation. Int J Pharm Res. 2020;12(3):568–75. http://dx.doi.org/10.31838/ijpr/2020.12.03.0.
13. Youssry I, Samy RM, AbdelMohsen M, Salama NM. The association between growth differentiation factor-15, erythroferrone, and iron status in thalassemic patients. Pediatr Res 2023. 2023 Jul 18;1–6. https://doi.org/10.1038/s41390-023-02729-5.
14. Shah FT, Porter JB, Sadasivam N, Kaya B, Moon JC, Velangi M, et al. Guidelines for the monitoring and management of iron overload in patients with haemoglobinopathies and rare anaemias. Br J Haematol. 2022 Jan 1;196(2):336–50. https://doi.org/10.1111/bjh.17839.
15. Sirbu O, Sorodoc V, Jaba IM, Floria M, Stoica A, Profire L, et al. The influence of cardiovascular medications on iron metabolism in patients with heart failure. Med. 2019;55(7):1–11. https://doi.org/10.3390/medicina55070329
16. Urmi SFH, Begum S, Munira FT, Das KC. Serum Calcium, Phosphate and Ferritin Level in Adult Male Patients with Transfusion Dependent Thalassemia. Bangabandhu Sheikh Mujib Med Coll J. 2023 Nov 20;2(2):97–100. http://dx.doi.org/10.3329/bsmmcj.v2i2.69841.
17. Saki F, Omrani GR. Evaluation of serum Fibroblast growth factor-23 in patients with betathalassemia major compared to healthy population. Iran J Pediatr Hematol Oncol. 2022;12(3):182–9. http://dx.doi.org/10.18502/ijpho.v12i3.10061.
18. Zhou C, Shi Z, Ouyang N, Ruan X. Hyperphosphatemia and Cardiovascular Disease. Front Cell Dev Biol. 2021 Mar 4;9. https://doi.org/10.3389%2Ffcell.2021.644363.
19. Yu U, Chen L, Wang X, Zhang X, Li Y, Wen F, et al. Evaluation of the vitamin D and biomedical statuses of young children with β-thalassemia major at a single center in southern China. BMC Pediatr . 2019 Oct 23;19(1):1–8. https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-019-1744-8.
20. Aguiar P, Cruz D, Rodrigues RF, Peixoto L, Araújo F, Ducla Soares JL. Hypocalcemic cardiomyopathy. Rev Port Cardiol (English Ed. 2013 Apr 1;32(4):331–5. http://www.revportcardiol.org/en-hypocalcemic-cardiomyopathy-articulo-S2174204913000597.
21. Baqi DH, Ahmed SF, Baba HO, Fattah FH, Salih AM, Ali RM, et al. Hypocalcemia as a cause of reversible heart failure: A case report and review of the literature. Ann Med Surg . 2022 May 1;77. https://doi.org/10.1016/j.amsu.2022.103572
22. Maes M, Moustafa SR, Al-Hakeim HK, Alhillawi ZH. In Transfusion-dependent Thalassemia, Increased Iron Overload is Associated with Lower Serum Alpha-klotho, Which is Strongly Associated with Lower Total and Ionized Calcium Concentrations. 2020;(July):1–31. https://doi.org/10.20944/preprints202007.0347.v1.
23. Cui W, Leng B, Wang G. Klotho protein inhibits H2O2-induced oxidative injury in endothelial cells via regulation of PI3K/AKT/Nrf2/HO-1 pathways. 2018; 97(5): 370–6. https://cdnsciencepub.com/doi/10.1139/cjpp-2018-0277.
24. Xie J, Yoon J, An SW, Kuro-o M, Huang CL. Soluble Klotho Protects against Uremic Cardiomyopathy Independently of Fibroblast Growth Factor 23 and Phosphate. J Am Soc Nephrol . 2015 May 1; 26(5): 1150–60. https://pubmed.ncbi.nlm.nih.gov/25475745.
25. Olejnik A, Franczak A, Krzywonos-Zawadzka A, Kałużna-Oleksy M, Bil-Lula I. The Biological Role of Klotho Protein in the Development of Cardiovascular Diseases. Biomed Res Int. 2018;2018. https://doi.org/10.1155/2018/5171945
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Ahmed J. Kadhim, Hedef D. El-Yaseen, Ali M. Jawad

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


