Correlation between Follicular Fluid Fatty Acids and Cell-Free Mitochondrial DNA in Women Undergoing Intra-Cytoplasmic Sperm Injections
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6642452Keywords:
Follicular Fluid, Fatty acids, Intracytoplasmic Sperm injection, Mitochondrial DNA, Oxidative StressAbstract
Background: Beta-oxidation of fatty acids takes place in the mitochondria to produce energy. This process is linked to the formation of free radicals. Previous researches propose that some fatty acids may be related to mitochondrial dysfunction, as they induce oxidative stress.
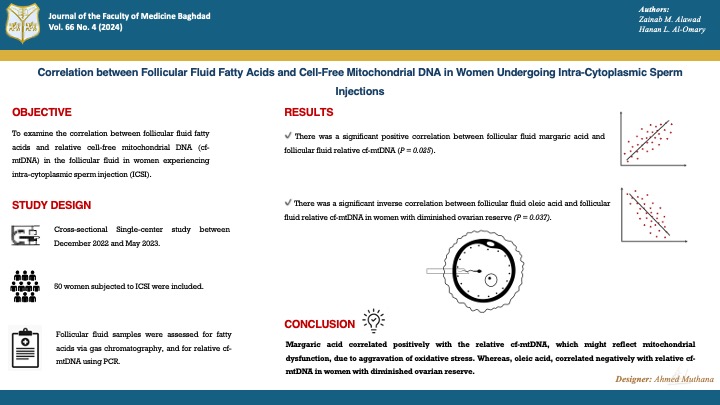
Objectives: To examine the correlation between follicular fluid fatty acids and relative cell-free mitochondrial DNA in the follicular fluid in women experiencing intra-cytoplasmic sperm injection (ICSI).
Methods: Fifty women subjected to ICSI participated in this cross-sectional research. Follicular fluid samples were obtained during oocyte pick-up. The samples were assessed for fatty acids, utilizing gas chromatography, and for relatively cell-free mitochondrial DNA, real-time polymerase chain reaction (PCR) was used.
Results: There was a strong significant positive correlation between follicular fluid margaric acid and follicular fluid relative to cell-free mitochondrial DNA, as the correlation coefficient was 0.869, and the P value was 0.025. In addition, a strong significant inverse correlation was noticed, in women with diminished ovarian reserve, between follicular fluid oleic acid and relative cell-free mitochondrial DNA in the follicular fluid, as indicated by a correlation coefficient = - 0.9 and a P value = 0.037.
Conclusion: Margaric acid correlated positively with the relative cell-free mitochondrial DNA, which might reflect mitochondrial dysfunction, due to aggravation of oxidative stress. Whereas, oleic acid, in women with diminished ovarian reserve, correlated negatively with relative cell-free mitochondrial DNA. However, more studies are required in this area of research.
Received: Aug. 2024
Revised: Oct. 2024
Accepted: Nov. 2024
Published: Dec. 2024
Downloads
References
Kadhum BS, Al- Shammaree SAW. Association of iron status in follicular fluid with pregnancy outcomes in infertile women undergoing IVF/ICSI. Iraqi J Sci. 2021;62(6):1779-86. https://doi.org/10.24996/ijs.2021.62.6.3.
Hanon MS, Mazhir SN, al-Ahmed HI, Haddad RA. Influence of non-thermal plasma (DBD) on infertility male semen with low sperm motility and DNA damage. Iraqi J Sci. 2022;63(4):1491-7. https://doi.org/10.24996/ijs.2022.63.4.9.
Salman FS, Al-Qadhi HI, Al Kareem BA. N-acetyl cysteine’s effect on semen parameters in a sample of Iraqi men with oligoasthenoteratozoospermia. J Fac Med Baghdad. 2022;64(3):170-4. https://doi.org/10.32007/jfacmedbagdad.6431938.
Ibrahim WW, Kadhim EJ, Abbas NS, Younis SR, Fawzi HA. Serological markers of autoimmunity in women with polycystic ovary syndrome. IJRPS. 2019;10(3):1746-50. https://doi.org/10.26452/ijrps.v10i3.1366.
Hamdi RA, Mohammed NS, AL-Naddawi AM. Determination of serum adiponectin levels in normal-weight women with polycystic ovary syndrome. J Fac Med Baghdad. 2015;57(2):175-8. https://doi.org/10.32007/jfacmedbagdad.572352.
Jasim RA, Umran MA, Humadi EH. Correlation between serum interleukins levels with anthropometric data and lipid profiles in obese Iraqi women with polycystic ovary syndrome. Iraqi J Sci. 2020;61(1):68-77. https://doi.org/10.24996/ijs.2020.61.1.7.
Shallal MM, Meran NM, Hussein ZA. Total L-carnitine and insulin resistance in non-obese and obese Iraqi women with polycystic ovary syndrome. J Fac Med Baghdad. 2023;65(1):20-6. https://doi.org/10.32007/jfacmedbagdad.6512040.
Aleqabi DS, Al-Qadhi HI. Tamoxifen vs. Letrozole as ovarian stimulants in infertile Iraqi women. IJDDT. 2021;11(4):1491-4. https://doi.org/10.25258/ijddt.11.4.64.
Ascar IF, Hameed AS. Serum prolactin, Preptin, CCL 18 and genetic polymorphisms in Iraqi women with polycystic ovary syndrome. Baghdad Sci J. 2021;18(4 (Suppl.)):1552-6. https://doi.org/10.21123/bsj.2021.18.4(Suppl.).1552.
Ghalib MM, Rasheed MK, Al-Naddawi AM. Association of Neuregulin-4 levels and body mass index with hyperandrogenism in Polycystic Ovary Syndrome patients. J Fac Med Baghdad. 2024;65(4):279-85. https://doi.org/10.32007/jfacmedbagdad.2140.
Yin J, Chang H-M, Li R, Leung PCK. Recent progress in the treatment of women with diminished ovarian reserve. GOCM. 2021;1(4):186-9. https://doi.org/10.1016/j.gocm.2021.10.004.
Koundouros N, Poulogiannis G. Reprogramming of fatty acid metabolism in cancer. Br J Cancer. 2020;122:4-22. https://doi.org/10.1038/s41416-019-0650-z.
Aparicio E, Martín-Grau C, Hernández-Martinez C, Voltas N, Canals J, Arija V. Changes in fatty acid levels (saturated, monounsaturated and polyunsaturated) during pregnancy. BMC Pregnancy Childbirth. 2021;21(778). https://doi.org/10.1186/s12884-021-04251-0.
Eidan SM, Khalil RI, Naser AF. Some fatty acid and semen characteristics of Holstein bulls as influenced by different sperm freez ability. Iraqi J Agric Sci. 2024;55(2):675-82. https://doi.org/10.36103/cg6xrf46.
Zeng X, Li S, Liu L, Cai S, Ye Q, Xue B, et al. Role of functional fatty acids in modulation of reproductive potential in livestock. J Animal Sci Biotechnol. 2023;14(24). https://doi.org/10.1186/s40104-022-00818-9.
Mirabi P, Chaichi MJ, Esmaeilzadeh S, Jorsaraei SGA, Bijani A, Ehsani M, et al. The role of fatty acids on ICSI outcomes: a prospective cohort study. Lipids Health Dis. 2017;16(18). https://doi.org/10.1186/s12944-016-0396-z.
Yenuganti VR, Viergutz T, Vanselow J. Oleic acid induces specific alterations in the morphology, gene expression and steroid hormone production of cultured bovine granulosa cells. Gen Comp Endocrinol. 2016;232:134-44. https://doi.org/10.1016/j.ygcen.2016.04.020.
Riley JS, Tait SW. Mitochondrial DNA in inflammation and immunity. EMBO Rep. 2020;21(4):e49799. https://doi.org/10.15252/embr.201949799.
Adhikari D, Lee I-w, Yuen WS, Carroll J. Oocyte mitochondria—Key regulators of oocyte function and potential therapeutic targets for improving fertility. Biol Reprod. 2022;106(2):366-77. https://doi.org/10.1093/biolre/ioac024.
Liu Y, Shen Q, Zhao X, Zou M, Shao S, Li J, et al. Cell-free mitochondrial DNA in human follicular fluid: a promising bio-marker of blastocyst developmental potential in women undergoing assisted reproductive technology. Reprod Biol Endocrinol. 2019;17(54). https://doi.org/10.1186/s12958-019-0495-6.
Taugourdeau A, Desquiret-Dumas V, Hamel JF, Chupin S, Boucret L, Ferré-L’Hotellier V, et al. The mitochondrial DNA content of cumulus cells may help predict embryo implantation. J Assist Reprod Genet. 2019;36(2):223-8. https://doi.org/10.1007/s10815-018-1348-5.
Talley JT, Mohiuddin SS. Biochemistry, fatty acid oxidation. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020. PMID: 32310462. https://europepmc.org/article/NBK/nbk556002.
Al-Rudaini AT, Al-Dujaily SS, Salih LA. A comparative study of preimplantation embryos development of young and aged mice treated with L-carnitine. Baghdad Sci J. 2024;21(6):1918-25. https://doi.org/10.21123/bsj.2023.8923.
Abdulsada HA, Taha EM. Nitric oxide, procalcitonin and oxidative stress index levels in acute bronchitis patients. J Fac Med Baghdad. 2024;66(2):129-34. https://doi.org/10.32007/jfacmedbagdad.6622257.
Jiang L, Yan J. The relationship between free fatty acids and mitochondrial oxidative stress damage to trophoblast cell in preeclampsia. BMC Pregnancy Childbirth. 2022;22(273). https://doi.org/10.1186/s12884-022-04623-0.
Xu Y, Wahlberg K, Love TM, Watson GE, Yeates AJ, Mulhern MS, et al. Associations of blood mercury and fatty acid concentrations with blood mitochondrial DNA copy number in the Seychelles Child Development Nutrition Study. Environ Int. 2019;124:278-83. https://doi.org/10.1016/j.envint.2019.01.019.
Hanon MS, Mazhir SN, Al-Ahmed HI, Hussein EA. Effect of cold atmospheric pressure plasma on DNA integrity in patients with asthenospermia. J Phys Conf Ser. 2019;1178:012029. https://doi.org/10.1088/1742-6596/1178/1/012029.
Alrawi QAT, Al-Issa YAH. The effect of recombinant FSH treatment on ceruloplasmin activity in infertility women undergoing IVF/ICSI. J Pharm Negat Results. 2022;13(special issue 08):1392-8. https://doi.org/10.47750/pnr.2022.13.S08.171.
Ishak GM, Feugang JM, Pechanova O, Pechan T, Peterson DG, Willard ST, et al. Follicular‐fluid proteomics during equine follicle development. Mol Reprod Dev. 2022;89(7):298-311. https://doi.org/10.1002/mrd.23622.
Al-Omary HL, Alawad ZM, Husseini B. Cell-free DNA as a clinical indicator in maternal blood. Turk J Endocrinol Metab. 2019;23(3):174-80. https://doi.org/10.25179/tjem.2019-65572.
The Rotterdam ESHRE/ASRM‐sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long‐term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41-7. https://doi.org/10.1093/humrep/deh098.
Hamdi RA, Abdul-Qahar ZH, Kadhum EJ, Alsaeed FA. Assessment of serum vitamin D levels in women with polycystic ovary syndrome. J Fac Med Baghdad. 2018;60(2):93-7. https://doi.org/10.32007/jfacmedbagdad.60212.
Fadhil NM, Hamdi RA. Evaluation of serum podocalyxin in Iraqi women with polycystic ovary syndrome. J Fac Med Baghdad. 2023;64(4):277-80. https://doi.org/10.32007/jfacmedbagdad.6441983.
Ferraretti AP, La Marca A, Fauser BCJM, Tarlatzis B, Nargund G, Gianaroli L; on behalf of the ESHRE working group on Poor Ovarian Response Definition. ESHRE consensus on the definition of ‘poor response' to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616-24. https://doi.org/10.1093/humrep/der092.
Jasim AH, Saleh BO, Al-Naddawi AM. Association between serum fructose level and insulin resistance in women with polycystic ovary syndrome: The effect of obesity. J Fac Med Baghdad. 2022;64(2):91-5. https://doi.org/10.32007/jfacmedbagdad.6421926.
Al-Rubae'i SHN, Naji TS, Turki KM, Edan DS. Association of the G/T rs4646 of CYP19 gene polymorphism with oxidative stress, vitamin A and estradiol in Iraqi women with endometriosis disease. Gene Rep. 2018;11:12-7. https://doi.org/10.1016/j.genrep.2018.01.005.
Abdlkarem HA, Zainulabdeen JA. A comparative study of vitamin D level and lactate dehydrogenase activity in relation to oxidative stress in women with osteoporosis. J Fac Med Baghdad. 2024;66(1):110-5. https://doi.org/10.32007/jfacmedbagdad.6612255.
Alawad ZM. Level of follicular fluid vitamin D and embryo quality in a sample of Iraqi women undergoing IVF. J Fac Med Baghdad. 2019;60(4):215-21. https://doi.org/10.32007/jfacmedbagdad.604758.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270-83. https://doi.org/10.1093/humrep/der037.
Mirabi P, Chaichi MJ, Esmaeilzadeh S, Jorsaraei SGA, Bijani A, Ehsani M. Does different BMI influence oocyte and embryo quality by inducing fatty acid in follicular fluid? Taiwan J Obstet Gynecol. 2017;56(2):159-64. https://doi.org/10.1016/j.tjog.2016.11.005.
Kermack AJ, Wellstead SJ, Fisk HL, Cheong Y, Houghton FD, Macklon NS, et al. The fatty acid composition of human follicular fluid is altered by a 6‐Week dietary intervention that includes marine omega‐3 fatty acids. Lipids. 2021;56(2):201-9. https://doi.org/10.1002/lipd.12288.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods. 2001;25(4):402-8. https://doi.org/10.1006/meth.2001.1262.
Srivastava A, Srivastava P, Mathur S, Mishra S, Abbas S, Gupta A, et al. Analysis of cellular and cell free mitochondrial DNA content and reactive oxygen species levels in maternal blood during normal pregnancy: a pilot study. BMC Pregnancy Childbirth. 2022;22(845). https://doi.org/10.1186/s12884-022-05156-2.
Čolak E, Pap D. The role of oxidative stress in the development of obesity and obesity-related metabolic disorders. J Med Biochem. 2021;40(1):1-9. https://doi.org/10.5937/jomb0-24652.
González F, Considine RV, Abdelhadi OA, Acton AJ. Oxidative stress in response to saturated fat ingestion is linked to insulin resistance and hyperandrogenism in polycystic ovary syndrome. J Clin Endocrinol Metab. 2019;104(11):5360-71. https://doi.org/10.1210/jc.2019-00987.
Meex RCR, Blaak EE. Mitochondrial dysfunction is a key pathway that links saturated fat intake to the development and progression of NAFLD. Mol Nutr Food Res. 2021;65(1):e1900942. https://doi.org/10.1002/mnfr.201900942.
Sun Y, Ge X, Li X, He J, Wei X, Du J, et al. High-fat diet promotes renal injury by inducing oxidative stress and mitochondrial dysfunction. Cell Death Dis. 2020;11(914). https://doi.org/10.1038/s41419-020-03122-4.
Prasun P. Mitochondrial dysfunction in metabolic syndrome. Biochim Biophys Acta Mol Basis Dis. 2020;1866(10):165838. https://doi.org/10.1016/j.bbadis.2020.165838.
Lemos GdO, Torrinhas RS, Waitzberg DL. Nutrients, physical activity, and mitochondrial dysfunction in the setting of metabolic syndrome. Nutrients. 2023;15(5):1217. https://doi.org/10.3390/nu15051217.
Huo P, Zhang N, Zhang P, Wu X. The levels of follicular fluid cell-free mitochondrial DNA could serve as a biomarker for pregnancy success in patients with small ovarian endometriosis cysts: A case-control study. Medicine (Baltimore). 2020;99(48):e23348. https://doi.org/10.1097/MD.0000000000023348.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Zainab M. Alawad, Hanan L. Al-Omary

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


