The Cytoprotective Effects of Melatonin on Gastric Ulcer: A Rat Model
DOI:
https://doi.org/10.32007/jfacmedbaghdad2467الكلمات المفتاحية:
Indomethacin، Melatonin، Rats، Stomach Ulcerالملخص
Background: Gastric ulcer is a prevalent gastrointestinal disorder caused by environmental factors and a higher intake of non-steroidal anti-inflammatory drugs (NSAIDs).
Objective: To investigate the prophylactic effects of melatonin on the histology, severity of gastric ulcers, and levels of inflammatory and oxidative stress markers (Interleukin-1beta (IL-1β) and Malondialdehyde (MDA)) in a rat model of indomethacin-induced ulcers.
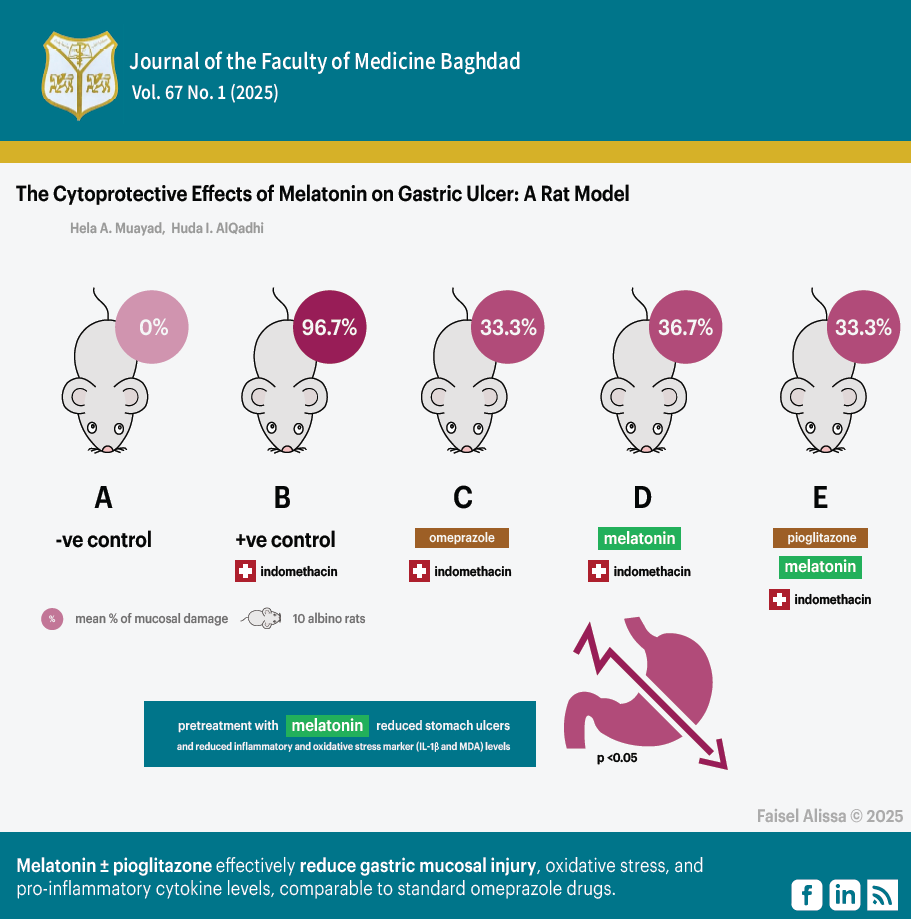
Methods: This study was performed at Al-Mustansiriyah University's Research Center for Cancer and Medical Genetics from November 2023 to May 2024. Fifty healthy male albino rats weighing between 150 - 250 grams were used. After 24 hours of fasting, these rats were divided into five groups, each with 10 rats. Group A: Received 1 ml of indomethacin vehicle (carboxymethylcellulose 1%) orally (negative control). Group B: Received 60 mg/ kg of indomethacin orally (positive control). Group C: Received 20 mg/ kg of omeprazole orally 30 minutes before indomethacin induction. Group D: Received 20 mg/ kg of melatonin solution orally 30 minutes before indomethacin induction. Group E: Received 30 mg/ kg of pioglitazone solution orally. After 1 hour, rats received a melatonin solution of 20 mg/ kg and waited for 30 minutes before induction.
Results: The group that received melatonin pretreatment at a dosage of 20 mg/kg exhibited a statistically significant reduction in the severity of stomach ulcers and histological damage score. The administration of melatonin at a dose of 20 mg/kg to the pre-treated group reduced inflammatory and oxidative stress markers (IL-1β and MDA) levels similar to those observed with the reference medication.
Conclusions: Melatonin alone or a combination of pioglitazone and melatonin effectively reduce gastric mucosal injury, oxidative stress, and pro-inflammatory cytokine levels, comparable to standard omeprazole drugs.
التنزيلات
المراجع
1. Imad R, Al-Qadh HI. The protective effects of Cilostazol on indomethacin-induced gastric ulcer in rat model. HIV Nurs. 2022;22(2):3578-83.
2. Dafalla SE, Alghamdi HYA, Alsaedi AM, Alzain MAI, Alsaedi ODA, Khormi MA, et al. Awareness of the general population in Jeddah about peptic ulcer disease. Int J Med Dev Ctries. 2021;5(2):656-62. https://doi.org/10.24911/IJMDC.51-1609363527.
3. Al-Marzooq TJ, Naji RE, Al-Majidi AK, Abbas Y. The use of serum Amylase as a predictive factor for mortality in Perforated Duodenal Ulcer. J Fac Med Baghdad. 2015;57(4):295-8. https://doi.org/10.32007/med.1936/jfacmedbagdad.v57i4.8.
4. Jahnavi K, Reddy PP, Vasudha B, Narender B. Non-steroidal anti-inflammatory drugs: an overview. J Drug Deliv Ther. 2019;9(1-s):442-8. https://doi.org/10.22270/jddt.v9i1-s.2287.
5. Ju Z, Li M, Xu J, Howell DC, Li Z, Chen FE. Recent development on COX-2 inhibitors as promising anti-inflammatory agents: The past 10 years. Acta Pharm Sin B. 2022;12(6):2790-807. https://doi.org/10.1016/j.apsb.2022.01.002.
6. Zhang M, Xia F, Xia S, Zhou W, Zhang Y, Han X, et al. NSAID-associated small intestinal injury: an overview from animal model development to pathogenesis, treatment, and prevention. Front Pharmacol. 2022;13:818877. https://doi.org/10.3389/fphar.2022.818877.
7. Matloub SYN, Manna MJ. The cytoprotective effect of different doses of Sildenafil on indomethacin-induced gastric mucosal damage in rats. J Fac Med Baghdad. 2010;52(4):426-31. https://doi.org/10.32007/jfacmedbagdad.524950.
8. Mohamed YT, Naguib IA, Abo-Saif AA, Elkomy MH, Alghamdi BS, Mohamed WR. Role of ADMA/DDAH-1 and iNOS/eNOS signaling in the gastroprotective effect of tadalafil against indomethacin-induced gastric injury. Biomed Pharmacother. 2022;150:113026. https://doi.org/10.1016/j.biopha.2022.113026.
9. Choudhary P, Roy T, Chatterjee A, Mishra VK, Pant S, Swarnakar S. Melatonin rescues swim stress induced gastric ulceration by inhibiting matrix metalloproteinase-3 via down-regulation of inflammatory signaling cascade. Life Sci. 2022;297:120426. https://doi.org/10.1016/j.lfs.2022.120426.
10. Matloub SYN. Captopril versus enalapril in the protection of the gastric mucosa against NSAID induced gastric mucosal injury in rats. J Fac Med Baghdad. 2011;53(2):236-40. https://doi.org/10.32007/jfacmedbagdad.532882.
11. Küçükler S, Kandemir FM, Yıldırım S. Protective effect of chrysin on indomethacin induced gastric ulcer in rats: role of multi-pathway regulation. Biotech Histochem. 2022;97(7):490-503. https://doi.org/10.1080/10520295.2021.2014569.
12. Panchal NK, Sabina EP. Non-steroidal anti-inflammatory drugs (NSAIDs): A current insight into its molecular mechanism eliciting organ toxicities. Food Chem Toxicol. 2023;172:113598. https://doi.org/10.1016/j.fct.2022.113598.
13. Rébé C, Ghiringhelli F. Interleukin-1β and cancer. Cancers (Basel). 2020;12(7):1791. https://doi.org/10.3390/cancers12071791.
14. Wang J, Liu H, Wang Y, Wu J, Wang C, Liu K, et al. The polymorphisms of interleukin-12B gene and susceptibility to inflammatory bowel diseases: a meta-analysis and trial sequential analysis. Immunol Invest. 2021;50(8):987-1006. https://doi.org/10.1080/08820139.2020.1863981.
15. Ajao AA, Sibiya NP, Moteetee AN. Sexual prowess from nature: A systematic review of medicinal plants used as aphrodisiacs and sexual dysfunction in sub-Saharan Africa. South African J Bot. 2019; 122:342-59. https://doi.org/10.1016/j.sajb.2018.08.011.
16. Chrustek A, Olszewska-Słonina D. Melatonin as a powerful antioxidant. Acta Pharm. 2021;71(3):335-54. https://doi.org/10.2478/acph-2021-0027.
17. Waleed S, Taha ATM, Uthman AT. Effect of Salivary Melatonin on Ionizing Radiation Worker and its Effect on Periodontal Disease. J Fac Med Baghdad. 2024;66(1):79-84. https://doi.org/10.32007/jfacmedbagdad.6612183.
18. Ivanov DO, Evsyukova II, Mironova ES, Polyakova VO, Kvetnoy IM, Nasyrov RA. Maternal melatonin deficiency leads to endocrine pathologies in children in early ontogenesis. Int J Mol Sci. 2021;22(4):2058. https://doi.org/10.3390/ijms22042058.
19. Bilici D, Süleyman H, Banoğlu ZN, Kiziltunç A, Avci B, Çiftçioğlu A, et al. Melatonin prevents ethanol-induced gastric mucosal damage possibly due to its antioxidant effect. Dig Dis Sci. 2002;47:856-61. https://doi.org/10.1023/A:1014764705864.
20. Morvaridzadeh M, Sadeghi E, Agah S, Nachvak SM, Fazelian S, Moradi F, et al. Effect of melatonin supplementation on oxidative stress parameters: a systematic review and meta-analysis. Pharmacol Res. 2020; 161:105210. https://doi.org/10.1016/j.phrs.2020.105210.
21. Ganguly K, Maity P, Reiter RJ, Swarnakar S. Effect of melatonin on secreted and induced matrix metalloproteinase‐9 and‐2 activity during prevention of indomethacin‐induced gastric ulcer. J Pineal Res. 2005;39(3):307-15. https://doi.org/10.1111/j.1600-079X.2005.00250.x.
22. Majumder R, Datta M, Chattopadhyay A, Bandyopadhyay D. Melatonin promotes gastric healing by modulating the components of matrix metalloproteinase signaling pathway: a novel scenario for gastric ulcer management. Melatonin Res. 2021;4(2):213-31. https://doi.org/10.32794/mr11250092.
23. Sánchez AB, Clares B, Rodríguez-Lagunas MJ, Fábrega MJ, Calpena AC. Study of melatonin as preventive agent of gastrointestinal damage induced by sodium diclofenac. Cells. 2020;9(1):180. https://doi.org/10.3390/cells9010180.
24. Bhatia A, Saikia PP, Dkhar B, Pyngrope H. Anesthesia protocol for ear surgery in Wistar rats (animal research). Anim Model Exp Med. 2022;5(2):183-8. https://doi.org/10.1002/ame2.12198.
25. Jafari A, Andishfar N, Esmaeilzadeh Z, Khezri MR, Ghasemnejad‐Berenji M. Gastroprotective effect of topiramate on indomethacin‐induced peptic ulcer in rats: Biochemical and histological analyses. Basic Clin Pharmacol Toxicol. 2022;130(5):559-68. https://doi.org/10.1111/bcpt.13718.
26. Nonaka H, Mino T, Sakamoto S, Oh JH, Watanabe Y, Ishikawa M, et al. Revisiting PFA-mediated tissue fixation chemistry: FixEL enables trapping of small molecules in the brain to visualize their distribution changes. Chem. 2023;9(2):523-40. https://doi.org/10.1016/j.chempr.2022.11.005.
27. Ekbbal R, Iqubal A, Ansari MA, Ahmad S, Haque SE. Evaluation of cardioprotective potential of isolated swerchirin against the isoproterenol-induced cardiotoxicity in wistar albino rats. Pharmacogn Mag. 2022;18(77). https://doi.org/10.4103/pm.pm_500_20.
28. Song H, Hou X, Zeng M, Chen X, Chen X, Yang T, et al. Traditional Chinese Medicine Li-Zhong-Tang accelerates the healing of indomethacin-induced gastric ulcers in rats by affecting TLR-2/MyD88 signaling pathway. J Ethnopharmacol. 2020;259:112979. https://doi.org/10.1016/j.jep.2020.112979.
29. Antonisamy P, Arasu MV, Dhanasekaran M, Choi KC, Aravinthan A, Kim NS, et al. Protective effects of trigonelline against indomethacin-induced gastric ulcer in rats and potential underlying mechanisms. Food Funct. 2016;7(1):398-408. https://doi.org/10.1039/C5FO00403A,
30. Maity P, Bindu S, Dey S, Goyal M, Alam A, Pal C, et al. Indomethacin, a non-steroidal anti-inflammatory drug, develops gastropathy by inducing reactive oxygen species-mediated mitochondrial pathology and associated apoptosis in gastric mucosa: a novel role of mitochondrial aconitase oxidation. J Biol Chem. 2009;284(5):3058-68. https://doi.org/10.1074/jbc.M805329200.
31. Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem Pharmacol. 2020;180:114147. https://doi.org/10.1016/j.bcp.2020.114147.
32. Lichtenberger LM, Zhou Y, Dial EJ, Raphael RM. NSAID injury to the gastrointestinal tract: evidence that NSAIDs interact with phospholipids to weaken the hydrophobic surface barrier and induce the formation of unstable pores in membranes. J Pharm Pharmacol. 2006;58(11):1421-8. https://doi.org/10.1211/jpp.58.10.0001.
33. Bindu S, Mazumder S, Dey S, Pal C, Goyal M, Alam A, et al. Nonsteroidal anti-inflammatory drug induces proinflammatory damage in gastric mucosa through NF-κB activation and neutrophil infiltration: Anti-inflammatory role of heme oxygenase-1 against nonsteroidal anti-inflammatory drug. Free Radic Biol Med. 2013;65:456-67. https://doi.org/10.1016/j.freeradbiomed.2013.07.027
34. Abdel-Tawab MS, Tork OM, Mostafa-Hedeab G, Hassan ME, Elberry DA. Protective effects of quercetin and melatonin on indomethacin induced gastric ulcers in rats. Reports Biochem Mol Biol. 2020;9(3):278. https://doi.org/10.29252/rbmb.9.3.278.
35. Konturek SJ, Konturek PC, Brzozowski T. Melatonin in gastroprotection against stress-induced acute gastric lesions and in healing of chronic gastric ulcers. J Physiol Pharmacol. 2006;57:51. https://pubmed.ncbi.nlm.nih.gov/17233075.
36. Celinski K, Konturek SJ, Konturek PC, Brzozowski T, Cichoz‐Lach H, Slomka M, et al. Melatonin or l‐tryptophan accelerates healing of gastroduodenal ulcers in patients treated with omeprazole. J Pineal Res. 2011;50(4):389-94. https://doi.org/10.1111/j.1600-079X.2011.00855.x.
37. Pal PK, Chattopadhyay A, Bandyopadhyay D. Functional interplay of melatonin in the bile duct and gastrointestinal tract to mitigate disease development: An overview. Melatonin Res. 2021;4(1):118-40. https://doi.org/10.32794/mr11250086
التنزيلات
منشور
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2025 Hela A. Muayad, Huda I. AlQadhi

هذا العمل مرخص بموجب Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


