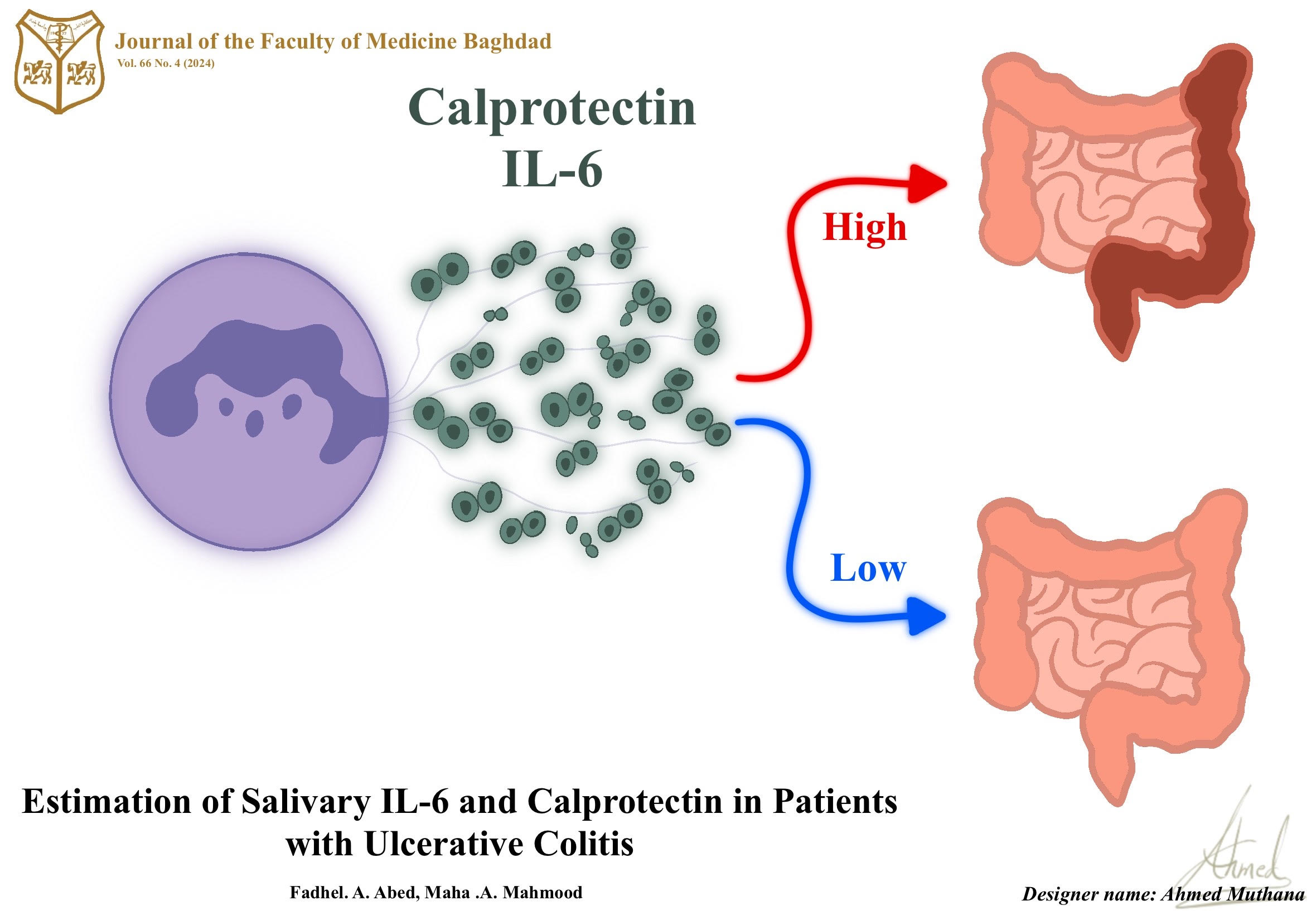
Estimation of Salivary IL-6 and Calprotectin in Patients with Ulcerative Colitis
DOI:
https://doi.org/10.32007/jfacmedbagdad.6612031Keywords:
Calprotectin, Inflammatory Bowel Diseases , Interleukin-6 , Saliva and Ulcerative ColitisAbstract
Background: Inflammatory bowel disease is chronic inflammation of the gastrointestinal tract it includes two condition; Crohn’s disease and ulcerative colitis. Calprotectin released by keratinocytes, phagocytes, monocytes, granulocytes and vascular cells is recognized by toll-like receptors (TLRs) to induce inflammatory response.
Objectives: In order to investigate if there are significant differences in the levels of those markers (IL6 and Calprotectin in between UC patients and healthy control subjects.
Patients and Methods: The subjects included were twenty-five patients with ulcerative colitis and twenty-five healthy individuals as the control group. All of whom ranged in age from 20-55 years, and the levels of interleukin-6 (IL-6) and Calprotectin in the saliva of UC patients were measured using the ELISA method
Result: When compared to the control group, the current findings indicated that both (IL-6) and Calprotectin levels were significantly higher in UC patients, (P=<0.05). Moreover, this study found a significant positive correlation between IL-6 levels and age in all study groups (UC and control) (P <0.05) and between IL-6 and Calprotectin in UC patients (p<0.05).
Conclusion: Higher levels of IL-6 and calprotectin in saliva of patients with UC disease as compared with healthy subjects (control) and as a result, both markers could be used as diagnostic markers for UC disease
Received: Feb. 2023
Revised: Jan. 2023
Accepted: Aug. 2023
Published: April 2024
Downloads
References
1. Abdul-Hussein SS, et al. Roles of IL-17A and IL-23 in the Pathogenesis of Ulcerative Colitis and Crohn’s Disease. Iraqi Journal of Science. 2021; 2526-2535. https://doi.org/10.24996/ijs.2021.62.8.5.
2. Frøslie KF, et al. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007; 133(2): 412-422. https://doi.org/10.1053/j.gastro.2007.05.05.
3. Manna MJ, Abu-Raghif A, Al-Saree OJAH. The value of doxycycline in acetic acid induce ulcerative colitis in rats. IJPSR. 2018; 9(8): 3567-3572. http://dx.doi.org/10.13040/IJPSR.0975-8232.9(8).3567-72.
4. Abdal-Zahra N, et al. The significance of miR-196a2 C< T single nucleotide polymorphism and serum levels of interleukin-1β (IL-1β) and interleukin-6 (IL-6) in colorectal cancer. JPharmSciRes. 2019; 11(4): 1652-165. https://doi.org/10.1016/j.mgene.2017.02.004.
5. Al-Hassan AA. Possible association of HLA class I and II molecules with Ulcerative colitis in Iraqi patients. Iraqi Journal of Medical Sciences. 2008; 6 (1).https://www.iasj.net/iasj/download/4cde74b676b80148
6. Daham KJ, Hamel KI, Khorsheed SA. Management of ulcerative colitis in a sample of Iraqi patients. International Journal of Surgery. 2019; 3(3):344-348. https://doi.org/10.33545/surgery.2019.v3.i3f.192.
7. Surcel M, et al. Inflammatory cytokine pattern is sex-dependent in mouse cutaneous melanoma experimental model. Journal of Immunology Research. 2017; 2017. https://doi.org/10.1155/2017/9212134.
8. Gabay C. Interleukin-6 and chronic inflammation. Arthritis research & therapy. 2006; 8(2): 1-6. https://doi.org/10.1186/ar1917
9. Juda TM, Beder S, Zaidan KI. Salivary Interleukine 6 and its role on developing periodentitis. Irq. Nat. J. Chem. 2016;16(1):22-31. https://injchemistry.uobabylon.edu.iq/index.php/chem/article/view/703/648
10. Larsen TB, et al. Platelets and anticoagulant capacity in patients with inflammatory bowel disease. Pathophysiology of Haemostasis and Thrombosis. 2002; 32(2): 92-96. https://doi.org/10.1159/000065082.
11. Al-Tameemi S, et al. Calprotectin may be positively associated with the severity of acne vulgaris. BJBiochemistry and Applied Biological Sciences. 2022; 3(02): 145-155. https://doi.org/10.47419/bjbabs.v3i02.124.
12. Wei L, Liu M, Xiong H. Role of calprotectin as a biomarker in periodontal disease. Mediators of Inflammation. 2019; 2019. https://doi.org/10.1155/2019/3515026.
13. Ostrowska L, et al. Which salivary components can differentiate metabolic obesity?. PLoS One. 2020; 15 (6): e0235358. https://doi.org/10.1371/journal.pone.0235358.
14. Gilat D. The best bound in the inequality of Hardy and Littlewood and its martingale counterpart. Proceedings of the American Mathematical Society. 1986; 97(3): 429-436. https://doi.org/10.1090/S0002-9939-1986-0840624-3
15. Hassan JT, Delmany AS. Epidemiological and clinical characteristics of patients with inflammatory bowel disease in Erbil City. Medical Journal of Babylon. 2018 Oct 1;15(4):281-5. https://doi.org/10.4103/MJBL.MJBL_65_18
16. Hammasur GA, Mohammed FO, Ahmad AJ. Assessment of rock slope stability along Sulaimaniyah-Qaradagh main road, near Dararash Village, Sulaimaniyah, NE-Iraq. Iraqi Journal of Science. 2020; 3266-3286. https://doi.org/10.24996/ijs.2020.61.12.15.
17. Hirano T. Interleukin 6 and its receptor: ten years later. International Reviews of Immunology. 1998; 16(3-4): 249-284. https://doi.org/10.3109/08830189809042997.
18. Atreya R, et al. Blockade of interleukin 6 trans signaling suppresses T-cell resistance against apoptosis in chronic intestinal inflammation: evidence in Crohn disease and experimental colitis in vivo. Nature Medicine. 2000; 6(5): 583-588. https://doi.org/10.1038/75068.
19. Baumann H, Gauldie J. The acute phase response. Immunology Today. 1994; 15(2): 74-80. https://doi.org/10.1016/0167-5699(94)90137-6.
20. Mazlam MZ, Hodgson HJ. Interrelations between interleukin-6, interleukin-1 beta, plasma C-reactive protein values, and in vitro C-reactive protein generation in patients with inflammatory bowel disease. Gut. 1994; 35(1): 77-83. https://doi.org/10.1136/gut.35.1.77.
21. Nielsen AA, et al. Saliva interleukin-6 in patients with inflammatory bowel disease. Scandinavian Journal of Gastroenterology. 2005; 40(12): 1444-1448. https://doi.org/10.1080/00365520510023774.
22. Al-Mudhaffer MH, Abdul-Ghafoor SH. Salivary assessment of interleukin-6, C-reactive protein, and albumin in ulcerative colitis patients in relation to oral findings. Journal of Baghdad College of Dentistry. 2013; 325(2204): 1-5. https://doi.org/10.12816/0014972.
23. Majster M, Almer S, Boström EA. Salivary calprotectin is elevated in patients with active inflammatory bowel disease. Archives of Oral Biology. 2019; 107: 104528. https://doi.org/10.1016/j.archoralbio.2019.104528.
24. Bjerke K, et al. Distribution of macrophages and granulocytes expressing L1 protein (Calprotectin) in human Peyer's patches compared with normal ileal lamina propria and mesenteric lymph nodes. Gut. 1993; 34(10): 1357-1363. https://doi.org/10.1136/gut.34.10.1357.
25. Fagerberg UL, et al. Fecal Calprotectin levels in healthy children studied with an improved assay. Journal of Pediatric Gastroenterology and Nutrition. 2003; 37(4): 468-472. https://doi.org/10.1097/00005176-200310000-00013.
26. Burak S, Margat J. Water management in the Mediterranean region: concepts and policies. Water Resources Management. 2016; 30(15): 5779-5797. https://doi.org/10.1007/s11269-016-1389-4.
27. Zhou HJ, et al. Validation of the functional assessment of cancer therapy-gastric module for the Chinese population. Health and Quality of Life Outcomes. 2012; 10(1): 1-8. https://doi.org/10.1186/1477-7525-10-145.
28. Shah SC, Khalili H, Gower-Rousseau C, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from western countries. Gastroenterology. 2018; 155: 1079–1089. https://doi.org/10.1053/j.gastro.2018.09.014.
29. Shah SC, Khalili H, Chen CY, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from the Asia-Pacific region. Aliment Pharmacol Ther. 2019; 49: 904–911. https://doi.org/10.1111/apt.15178.
30. Nijakowski K, Surdacka A. Salivary Biomarkers for Diagnosis of Inflammatory Bowel Diseases: A Systematic Review. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21207477.
31. Nijakowski K, Surdacka A. Salivary Biomarkers for Diagnosis of Inflammatory Bowel Diseases: A Systematic Review. Int J Mol Sci. 2020; 21:7477. https://doi.org/10.3390/ijms21207477.
32. Szczeklik K, Owczarek D, Pytko-Polónczyk J, Kęsek B, Mach TH. Proinflammatory Cytokines in the Saliva of Patients with Active and Non-Active Crohn’s Disease. Pol Arch Med Wewn. 2012; 122:200-208. https://doi.org/10.20452/pamw.1256.
33. Dobre M, et al. Differential Intestinal Mucosa Transcriptomic Biomarkers for Crohn’s Disease and Ulcerative Colitis. Journal of Immunology Research. 2018. https://doi.org/10.1155/2018/9208274.
Downloads
Additional Files
Published
Issue
Section
License
Copyright (c) 2024 Fadhel A. Abed, Maha A. Mahmood

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


