The Total Antioxidant Capacity and its Relationship with Atherosclerosis Risk Factors in a Sample of Iraqi Individuals with Type 2 Diabetes Mellitus
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632334Keywords:
Antioxidant, Diabetes Mellitus Type 2, Glycated Hemoglobin, Malondialdehyde, Oxidative stressAbstract
Background: Diabetes mellitus is significantly related to cardiovascular disease, such as atherosclerosis. Antioxidants are essential in the prevention of atherosclerosis by a variety of mechanisms, which encompass the suppression of free radical production, inhibition of low-density lipoprotein oxidation, and prevention of atherosclerotic plaque formation.
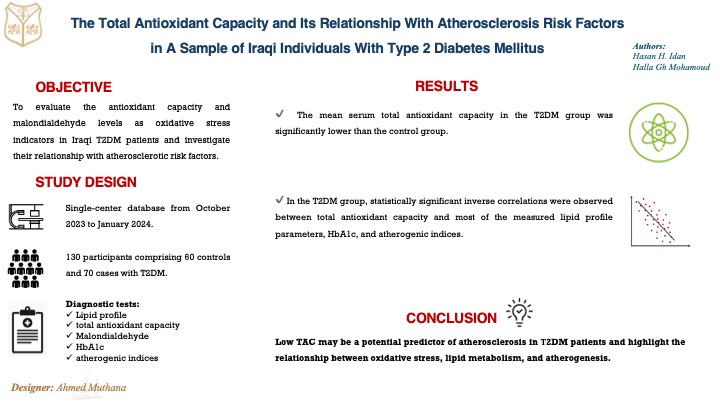
Objectives: This study aims to evaluate the levels of total antioxidant capacity and malondialdehyde as oxidative stress indicators in Iraqi type 2 diabetes mellitus (T2DM) patients and investigate their relationship with atherosclerotic risk factors.
Methods: This case-control study took place between October 2023 to January 2024 at Al-Karkh General Hospital in Baghdad. The study included a total of 130 participants: 70 individuals diagnosed with T2DM and 60 healthy controls were recruited from relatives of patients attending the hospital and hospital employees who did not have T2DM. The two study groups were age-matched. Blood samples from both groups were analyzed to determine the following parameters: Lipid profile, total antioxidant capacity (TAC), Malondialdehyde (MDA) as an oxidative stress marker, glycated hemoglobin (HbA1c), and atherogenic indices (e.g. atherogenic index of plasma).
Results: The mean serum total antioxidant capacity (TAC) in the T2DM group was significantly lower than the control group (46.9 ± 5.05 U/mL vs. 70.8 ± 4.71 U/mL). This indicates a highly significant difference between the groups. Additionally, in the T2DM group, statistically significant inverse correlations were observed between TAC and most of the measured lipid profile parameters, HbA1c, and atherogenic indices.
Conclusions: Low TAC may be a potential predictor of atherosclerosis in Τ2DM patients and highlight the relationship between oxidative stress, lipid metabolism, and thermogenesis.
Received: Feb. 2024
Revised: Jul. 2024
Accepted: Jul. 2024
Downloads
References
Al-Yassin H. Correlation of Serum levels of Chromium, Copper, and Manganese with the Glucose levels in Type 2 Diabetes Mellitus in Iraq. Journal of the Faculty of Medicine Baghdad. 2024;65(4). https://doi.org/10.32007/jfacmedbagdad.2126 .
Hassan ZM, Hamdi RA, Al Bassam EN. Evaluation of the Role of Serum Malondialdehyde in the Pathogenesis of Diabetic Retinopathy. JFacMed Baghdad. 2022; 64 (3):1958. https://doi.org/10.32007/jfacmedbagdad.6431957
Abdullateef AH, Saleh B. Evaluation of glycated hemoglobin results in different anticoagulant materials and methods. MJB. 2021;18(4): 351. https://doi.org/10.4103/MJBL.MJBL_49_21
Mansour AA, Alibrahim NT, Alidrisi HA, Alhamza AH, Almomin AM, Zaboon IA, et al. Prevalence and correlation of glycemic control achievement in patients with type 2 diabetes in Iraq: A retrospective analysis of a tertiary care database over a 9-year period. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(3):265-72. https://doi.org/10.1016/j.dsx.2020.03.008
Björkegren JLM, Lusis AJ. Atherosclerosis: Recent developments. Cell. 2022;185(10):1630-45.
https://doi.org/10.1016/j.cell.2022.04.004
Khalid MM, Nader MI, Mahood RAH. Evaluation of oxidative stress in idiopathic male infertility in the Iraqi population. Biomedicine. 2023;43(02):615-20. https://doi.org/10.51248/.v43i02.2534
Yuan K, Zhang Y. Oxidative Stress and Antioxidant Strategies in Human Diseases. Oxidative Stress: Human Diseases and Medicine. 2021:1-26. https://doi.org/10.1007/978-981-16-0522-2_1
Poznyak AV, Grechko AV, Orekhova VA, Chegodaev YS, Wu W-K, Orekhov AN. Oxidative stress and antioxidants in atherosclerosis development and treatment. Biology. 2020;9(3):60.
https://doi.org/10.3390/biology9030060
Chang X, Zhang T, Zhang W, Zhao Z, Sun J. Natural drugs as a treatment strategy for cardiovascular disease through the regulation of oxidative stress. Oxidative Medicine and Cellular Longevity. 2020. https://doi.org/10.1155/2020/5430407
Silvestrini A, Meucci E, Ricerca BM, Mancini A. Total antioxidant capacity: biochemical aspects and clinical significance. International Journal of Molecular Sciences. 2023;24(13):10978. https://doi.org/10.3390/ijms241310978
Garcia C, Blesso CN. Antioxidant properties of anthocyanins and their mechanism of action in atherosclerosis. Free Radical Biology and Medicine. 2021; 172:152-66. https://doi.org/10.1016/j.freeradbiomed.2021.05.040
Varadhan S, Venkatachalam R. Evaluation of oxidative stress parameters and antioxidant status in coronary artery disease patients. Archives of Razi Institute. 2022;77(2):853.
https://doi.org/10.22092%2FARI.2022.357069.1965
Azzal HS, Majeed MJ, Allawi AAD, Hammoudi FA. Correlation of Soluble Klotho with Progress Stages of Diabetic Nephropathy. Biochemical & Cellular Archives. 2021;21(1). https://connectjournals.com/03896.2021.21.1585
Karkoush HG, Saifullah PH. Energy Level and Oxidative Stress Status in Cardiovascular Disease. Journal of Medicinal and Chemical Sciences. 2023;6(2):449-57.
https://www.sid.ir/paper/1140366/en
Mousa RF. Evaluation of Antioxidants Capacity of Non-Enzymatic Antioxidants and Its Effect in Glucose Level in Diabetic Patients. Indian Journal of Forensic Medicine & Toxicology. 2021;15(1). https://doi.org/10.37506/ijfmt.v15i1.13781
Yarube IU, Gwarzo IM. Cognitive impairment and reduced antioxidant capacity in patients with type 2 diabetes. Sahel Medical Journal. 2019;22(4):171.
https://doi.org/10.4103/smj.smj_37_18
Mehri H, Aslanabadi N, Nourazarian A, Shademan B, khaki‐khatibi F. Evaluation of the serum levels of Mannose binding lectin‐2, tenascin‐C, and total antioxidant capacity in patients with coronary artery disease. Journal of Clinical Laboratory Analysis. 2021;35(10):e23967.
https://doi.org/10.1002/jcla.23967
Leopold JA. Antioxidants and coronary artery disease: from pathophysiology to preventive therapy. Coronary artery disease. 2015;26(2):176.
https://doi.org/10.1097/MCA.0000000000000187
Kumar S, Kumar A, Khan MM. Estimation of aldose reductase activity and malondialdehyde levels in patients with type 2 diabetes mellitus. Biomedical and Pharmacology Journal. 2019;12(2):1001-7. https://doi.org/10.13005/bpj/1728
Mahreen R, Mohsin M, Nasreen Z, Siraj M, Ishaq M. Significantly increased levels of serum malonaldehyde in type 2 diabetics with myocardial infarction. International journal of diabetes in developing countries. 2010;30(1):49. https://doi.org/10.4103/0973-3930.60006
Mazzone T, Chait A, Plutzky J. Cardiovascular disease risk in type 2 diabetes mellitus: insights from mechanistic studies. The Lancet. 2008;371(9626):1800-9.
https://doi.org/10.1016/S0140-6736(08)60768-0
Borggreve S, De Vries R, Dullaart R. Alterations in high‐density lipoprotein metabolism and reverse cholesterol transport in insulin resistance and type 2 diabetes mellitus: role of lipolytic enzymes, lecithin: cholesterol acyltransferase and lipid transfer proteins. European journal of clinical investigation. 2003;33(12):1051-69. https://doi.org/10.1111/j.1365-2362.2003.01263.x
Krauss RM. Lipids and lipoproteins in patients with type 2 diabetes. DiaCare. 2004;27(6):1496-504. https://doi.org/10.2337/diacare.27.6.1496
Zheng D, Li H, Ai F, Sun F, Singh M, Cao X, et al. Association between the triglyceride to high-density lipoprotein cholesterol ratio and the risk of type 2 diabetes mellitus among Chinese elderly: the Beijing Longitudinal Study of Aging. BMJ Open Diabetes Research & Care. 2020;8(1). https://doi.org/10.1136/bmjdrc-2019-000811
Ye S, Ran H, Zhang H, Wu H, Li W, Du S, et al. Elevated serum triglycerides are associated with ketosis-prone type 2 diabetes in young individuals. Diabetes, Metabolic Syndrome and Obesity. 2021:497-504. https://doi.org/10.2147/DMSO.S296085
Zhang B-H, Yin F, Qiao Y-N, Guo S-D. Triglyceride and triglyceride-rich lipoproteins in atherosclerosis. Frontiers in Molecular Biosciences. 2022;9:909151.
https://doi.org/10.3389/fmolb.2022.909151
Chait A, Ginsberg HN, Vaisar T, Heinecke JW, Goldberg IJ, Bornfeldt KE. Remnants of the triglyceride-rich lipoproteins, diabetes, and cardiovascular disease. Diabetes. 2020;69(4):508-16.
https://doi.org/10.2337/dbi19-0007
Kuusisto S, Holmes MV, Ohukainen P, Kangas AJ, Karsikas M, Tiainen M, et al. Direct estimation of HDL-mediated cholesterol efflux capacity from serum. Clinical chemistry. 2019;65(8):1042-50. https://doi.org/10.1373/clinchem.2018.299222
Casula M, Colpani O, Xie S, Catapano AL, Baragetti A. HDL in atherosclerotic cardiovascular disease: in search of a role. Cells. 2021;10(8):1869.
https://doi.org/10.3390/cells10081869
Ahmadi A, Jamialahmadi T, Sahebkar A. Polyphenols and atherosclerosis: A critical review of clinical effects on LDL oxidation. Pharmacological Research. 2022:106414.
https://doi.org/10.1016/j.phrs.2022.106414
Huang J, Lin H, Wang S, Li M, Wang T, Zhao Z, et al. Association between serum LDL‐C concentrations and risk of diabetes: A prospective cohort study. Journal of Diabetes. 2023;15(10):881-9. https://doi.org/10.1111/1753-0407.13440
Taskinen MR, Björnson E, Matikainen N, Söderlund S, Pietiläinen KH, Ainola M, et al. Effects of liraglutide on the metabolism of triglyceride‐rich lipoproteins in type 2 diabetes. Diabetes, obesity and metabolism. 2021;23(5):1191-201. https://doi.org/10.1111/dom.14328
Acar O, Sarac GA, Rota DD, Aksoy H. Evaluation of pro‐atherogenic lipid profile and high atherohenic indexes in patients with Behçet's disease: A case-control study. Journal of Cosmetic Dermatology. 2023. https://doi.org/10.1111/jocd.15647
Fu L, Zhou Y, Sun J, Zhu Z, Xing Z, Zhou S, et al. Atherogenic index of plasma is associated with major adverse cardiovascular events in patients with type 2 diabetes mellitus. Cardiovascular diabetology. 2021;20(1):1-11.
https://doi.org/10.1186/s12933-021-01393-5
Prabandari NPSS, Wirawati IAP, Mahartini NN. Relationship between atherogenic index of plasma with HbA1c levels in type 2 diabetes mellitus patients. IJCPML. 2021;28(1):71-4.
https://doi.org/10.24293/ijcpml.v28i1.1743
Widanagamage R, Silva K, Ayeshmantha H, Kariyawasam K, Wijesinghe R. Correlation of Atherogenic Index of Plasma and Atherogenic Coefficient with Cardiovascular Disease Risk assessed by ASCVD Risk Calculator. JHSIR. 2023;4(01). https://doi.org/10.31357/jhsir.v4i01.6329
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Hasan H. Idan, Halla G. Mohamoud

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


