Evaluation of Metanephrine and Lactate Dehydrogenase in Pediatric Wilms Tumor and Neuroblastom
DOI:
https://doi.org/10.32007/jfacmedbaghdad3143Keywords:
Lactate Dehydrogenase, Metanephrine, Neuroblastoma, Pediatric cancer, Wilms tumorAbstract
Background: Wilms' tumor and Neuroblastoma are common pediatric malignancies, with biochemical markers like plasma metanephrines and serum lactate dehydrogenase (LDH) being studied for diagnostic and prognostic values. Metanephrine, a catecholamine metabolite, is elevated in Neuroblastoma due to tumor secretion. Elevated LDH levels may correlate with tumor burden and indirectly indicate disease activity.
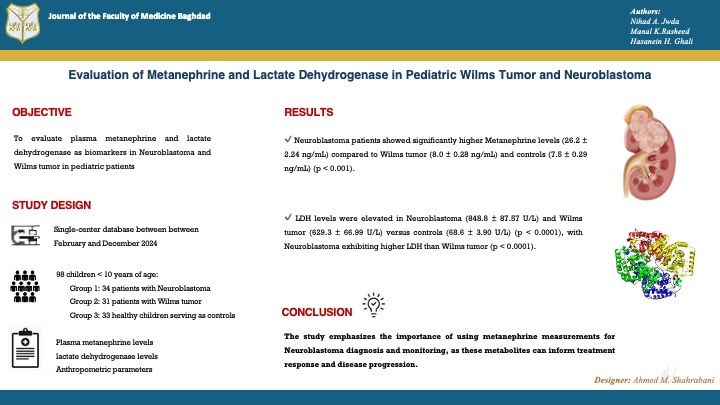
Objectives: To evaluate plasma metanephrine and lactate dehydrogenase as biomarkers in Neuroblastoma and Wilms tumor in pediatric patients.
Methods: The study was conducted between February and December 2024, in the Children Welfare Teaching Hospital, Medical City Complex, Baghdad, Iraq, and the Department of Biochemistry, College of Medicine, University of Baghdad. A Total of 98 children under the age of 10 years were included and grouped into: Group 1: 34 patients with Neuroblastoma, Group 2: 31 patients with Wilms tumor, and Group 3: 33 healthy children serving as controls. Blood samples (5 mL) were collected from all participants. Plasma metanephrine levels were measured using an ELISA method, while lactate dehydrogenase levels were determined using the Roche Cobas analyzer. Anthropometric parameters were also measured.
Results: The study found no significant differences in age, weight, or height among Neuroblastoma, Wilms tumor, and control groups. However, Neuroblastoma patients showed significantly higher Metanephrine levels (26.2 ± 2.24 ng/mL) compared to Wilms tumor (8.0 ± 0.28 ng/mL) and controls (7.5 ± 0.29 ng/mL) . Similarly, LDH levels were elevated in Neuroblastoma (848.8 ± 87.57 U/L) and Wilms tumor (629.3 ± 66.99 U/L) versus controls (68.6 ± 3.90 U/L), with Neuroblastoma exhibiting higher LDH than Wilms tumor.
Conclusion: The study emphasizes the importance of using metanephrine measurements for Neuroblastoma diagnosis and monitoring, as these metabolites can inform treatment response and disease progression. Neuroblastoma exhibits higher levels of metanephrine and lactate dehydrogenase, indicating a larger tumor burden. Wilms tumor does not share these characteristics.
Received: April 2025
Revised: July 2025
Accepted: Aug. 2025
Published Online: Aug. 2025
Published: Oct 2025
References
1.Nong J, Su C, Li C, Wang C, Li W, Li Y, et al. Global, regional, and national epidemiology of childhood neuroblastoma (1990-2021): a statistical analysis of incidence, mortality, and DALYs. EClinicalMedicine. 2025;79.https://doi.org/10.1016/j.eclinm.2024.102964.
2. Lanza C, Galeazzi V, Carboni N, De Berardinis A, De Marino L, Barile A, et al. Neuroblastoma image-defined risk factors in adrenal neuroblastoma: role of radiologist. Gland Surg. 2019;8(Suppl 3):S168. https://doi.org/10.21037/gs.2019.06.01.
3. Heck JE, Ritz B, Hung RJ, Hashibe M, Boffetta P. The epidemiology of neuroblastoma: a review. Paediatr Perinat.
https://doi.org/10.1111/j.1365-3016.2008.00983.x.
4. Perrotta G, Castellani D. Wilms Tumor: Updates about Pathogenesis and New Possible Clinical Treatments of the Most Frequent Pediatric Urogenital Cancer: A Narrative Review. Surgeries. 2023;4(4):678-97. https://doi.org/10.3390/surgeries4040064.
5. Espinoza AF, Onwuka E, Siegel DA, Dai S, Vasudevan SA, Scheurer ME, et al. Incidence and Survival of Children and Adolescents With Wilms Tumor, United States, 2001-2020. Cancer Med. 2025;14(3):e70598.
https://doi.org/10.1002/cam4.70598.
6. Neagu MC, David VL, Iacob ER, Chiriac SD, Muntean FL, Boia ES. Wilms' Tumor: A Review of Clinical Characteristics, Treatment Advances, and Research Opportunities. Medicina (B Aires). 2025;61(3):491.
https://doi.org/10.3390/medicina61030491.
7. Paravati S, Rosani A, Warrington SJ. Physiology, catecholamines. In: StatPearls [Internet]. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK507716/.
8. Vavřínová A, Behuliak M, Vaněčková I, Zicha J. The abnormalities of adrenomedullary hormonal system in genetic hypertension: their contribution to altered regulation of blood pressure. Physiol Res. 2021;70(3):307.
https://doi.org/10.33549/physiolres.934687.
9. Chu B, Marwaha K, Sanvictores T, Awosika AO, Ayers D. Physiology, stress reaction. In: StatPearls [Internet]. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK541120/.
10. Eisenhofer G, Deutschbein T, Constantinescu G, Langton K, Pamporaki C, Calsina B, et al. Plasma metanephrines and prospective prediction of tumor location, size and mutation type in patients with pheochromocytoma and paraganglioma. Clin Chem Lab Med. 2021;59(2):353-63. https://doi.org/10.1515/cclm-2020-0904
11. Harding M, Deyell RJ, Blydt-Hansen T. Catecholamines in neuroblastoma: Driver of hypertension, or solely a marker of disease? Cancer reports (Hoboken, NJ). 2022 Aug;5(8):e1569. https://doi.org/10.1002/cnr2.1569
12. Hussain MF, Alwan AF, Fahad HI, Saeed SR. Serum Lactate Dehydrogenase Level in Acute Leukemias. J Fac Med Baghdad [Internet]. 2008;49(4):369-74. Available from: https://doi.org/10.32007/jfacmedbagdad.4941323.
13. Chen X, Liu L, Kang S, Gnanaprakasam JNR, Wang R. The lactate dehydrogenase (LDH) isoenzyme spectrum enables optimally controlling T cell glycolysis and differentiation. Sci Adv. 2023;9(12):eadd9554. https://doi.org/10.1126/sciadv.add9554.
14. A. Abdlkarem H, A. Zainulabdeen J. A Comparative Study of Vitamin D Level and Lactate Dehydrogenase Activity in Relation to Oxidative Stress in Women with Osteoporosis. J Fac Med Baghdad [Internet]. 2024;66(1):110-5. Available from: https://doi.org/10.32007/jfacmedbagdad.6612255.
15. Moroz V, Machin D, Hero B, Ladenstein R, Berthold F, Kao P, et al. The prognostic strength of serum LDH and serum ferritin in children with neuroblastoma: a report from the International Neuroblastoma Risk Group (INRG) project. Pediatr Blood Cancer. 2020;67(8):e28359. https://doi.org/10.1002/pbc.28359.
16. Peitzsch M, Butch ER, Lovorn E, Mangelis A, Furman WL, Santana VM, et al. Biochemical testing for neuroblastoma using plasma free 3-O-methyldopa, 3-methoxytyramine, and normetanephrine. Pediatr Blood Cancer. 2020 Feb;67(2):e28081. https://doi.org/10.1002/pbc.28081
17. de Carvalho LG, Kobayashi T, Cypriano M dos S, Caran EMM, Lederman HM, Alves MT de S, et al. Diagnostic errors in Wilms' tumors: Learning from our mistakes. Front Pediatr. 2021;9:757377. https://doi.org/10.3389/fped.2021.757377
18. Aminzadeh S, Vidali S, Sperl W, Kofler B, Feichtinger RG. Energy metabolism in neuroblastoma and Wilms tumor. Transl Pediatr. 2015;4(1):20. https://doi.org/10.3978/j.issn.2224-4336.2015.01.04.
19. Dorneburg C, Fischer M, Barth TFE, Mueller-Klieser W, Hero B, Gecht J, et al. LDHA in neuroblastoma is associated with poor outcome and its depletion decreases neuroblastoma growth independent of aerobic glycolysis. Clin Cancer Res. 2018;24(22):5772-83. https://doi.org/10.1158/1078-0432.CCR-17-2578.
20. Kunc M, Gabrych A, Dulak D, Hasko K, Styczewska M, Szmyd D, et al. Systemic inflammatory markers and serum lactate dehydrogenase predict survival in patients with Wilms tumour. Arch Med Sci AMS. 2021;18(5):1253. https://doi.org/10.3389/fped.2021.757377
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Nihad A. Jwda, Manal K. Rasheed , Hasanein H.Ghali

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


