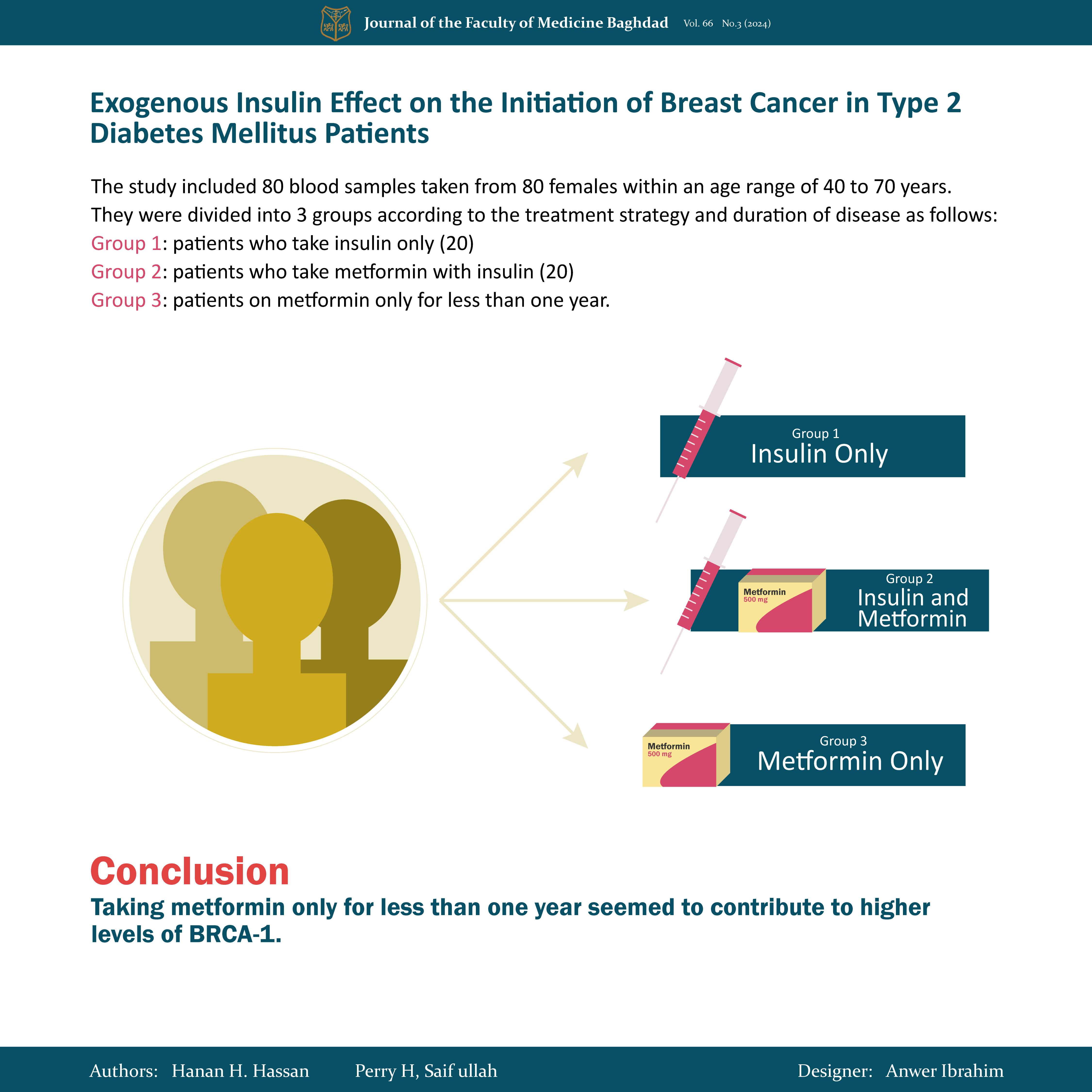
Exogenous Insulin Effect on the Initiation of Breast Cancer in Type 2 Diabetes Mellitus Patients
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632324Keywords:
BRCA1 protein, Breast cancer, Estrogen receptor alpha, Insulin, Type 2 diabetes mellitusAbstract
Background: Growing evidence has indicated that women with type 2 diabetes mellitus are at an increased risk of developing breast cancer. However, as a major adjuvant treatment, the influence of hormone therapy such as exogenous insulin on type 2 diabetes mellitus in primary breast-cancer remains controversial.
Objective: To explore the relationship between different types of hypoglycemic medications for diabetes and the factors that may contribute to the initiation of breast cancer.
Methods: The study included 80 blood samples taken from 80 females recruited from Ibn Al-Bitar Center for Cardiac Surgery Hospital in Baghdad, Iraq, between November 2022 and February 2023. They were within the age range of 40 to 70 years. They were divided into three groups according to the treatment strategy and duration of disease as follows: Group 1: (20) patients who take insulin only, Group 2: (20) patients who take metformin with insulin, and G 3: (40) patients on metformin only for less than one year. An enzymatic oxidation technique was used to test the following biochemical parameters for all research groups: Total cholesterol, triglycerides, fasting blood glucose, and high-density lipoprotein cholesterol. Using the Friedewald formula, the very low-density lipoprotein cholesterol and low-density lipoprotein cholesterol were determined. Using an enzymatic process, Insulin levels and Insulin like growth factor-1(IGF-1), Estrogen receptor alpha (ERα) levels, and breast cancer susceptibility protein 1 (BRCA1) were measured with an enzyme-linked immunosorbent assay (ELISA). Glycated hemoglobin (HbA1c) level was measured with a sandwich immunodetection method. Finally, The Homeostasis Model Assessment for insulin resistance (HOMA-IR) was calculated according to the specific formula.
Results: The values for HbA1C%, FBS, and lipid profile showed non-significant differences when compared between study groups. While BRCA-1, estrogen receptor alpha (ERα), insulin, insulin growth factor IGF-1, and HOMA IR All showed significant differences among all groups.
Conclusion: Taking metformin only for less than one year seemed to contribute to higher levels of BRCA-1.
Received: Feb. 2024
Revised: Jun. 2024
Accepted: July 2024
Published: Oct .2024
Downloads
References
Sadeghi A, Niknam M, Momeni-Moghaddam MA, Shabani M, Aria H, Bastin A, et al. Crosstalk between autophagy and insulin resistance: evidence from different tissues. Eur JMR. 2023; 28(1):456. https://doi.org/10.1186/s40001-023-01424-9.
Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. The lancet. 2017; 389 (10085): 2239-51. (17)30058-2. https://doi.org/10.1016/S0140-6736
Hameed AS, Khaleel FM, Rahma AM. The response of acromegalic patients (Diabetic versus non-diabetic) to Long-acting-repeatable Octreotide (LAR) in the presence or absence of Glutathion S transferase (GSTM1, GSTT1) Genes. JPharmaSR. 2019; 11(2):495-500.URL
Łukasiewicz S, Czeczelewski M, Forma A, Baj J, Sitarz R, Stanisławek A. Breast cancer—epidemiology, risk factors, classification, prognostic markers, and current treatment strategies—an updated review. Cancers. 202;13(17):4287 . https://doi.org/10.3390/cancers13174287.
Ali SE, Khaleel FM. Assessing the Activity of Renin and GST in the Serum of Ladies Suffering from Polycystic Ovary Syndrome and COVID-19 to Predict the Danger of Cardiac Disease. BSJ. 2023; 20(3) (Suppl.): 0986. https://doi.org/10.21123/bsj.2023.7879.
Rahmani J, Montesanto A, Giovannucci E, Zand H, Barati M, Kopchick JJ, et al. Association between IGF‐1 levels ranges and all‐cause mortality: A meta‐analysis. Aging Cell. 2022; 21(2): e13540. https://doi.org/10.1111/acel.13540.
Díaz del Moral S, Benaouicha M, Muñoz-Chápuli R, Carmona R. The insulin-like growth factor signalling pathway in cardiac development and regeneration. IJMS Journa. 2021 26;23(1):234. https://doi.org/10.3390/ijms23010234.
Wondmkun YT. Obesity, insulin resistance, and type 2 diabetes: associations and therapeutic implications. DMSO. 2020:3611-6. https://doi.org/10.2147/DMSO.S275898.
Mustafa SA, Hasan BF, Ibrahim N. Estimation of ferritin, erythropoietin in obese Iraqi type II diabetic patients. BCA. 2019;19(2):3307-12. http://dx.doi.org/10.35124/bca.2019.19.2.3307.
Baker C, Retzik-Stahr C, Singh V, Plomondon R, Anderson V, Rasouli N. Should metformin remain the first-line therapy for treatment of type 2 diabetes?. TAEM. 2021; https://doi.org/10.1177/2042018820980225.
Samuel SM, Varghese E, Kubatka P, Triggle CR, Büsselberg D. Metformin: the answer to cancer in a flower? Current knowledge and future prospects of metformin as an anti-cancer agent in breast cancer. Biom. 2019; 9(12):846. https://doi.org/10.3390/biom9120846.
Gholami M, Klashami ZN, Ebrahimi P, Mahboobipour AA, Farid AS, Vahidi A, et al. Metformin and long non-coding RNAs in breast cancer. JTM. 2023; 21(1):155. https://doi.org/10.1186/s12967-023-03909-x
Xue L, Chen F, Yue F, Camacho L, Kothapalli S, Wei G, et al. Metformin and an insulin/IGF-1 receptor inhibitor is synergistic in blocking growth of triple-negative breast cancer. Breast cancer research and treatment. 2021; 185: 73-84. https://doi.org/10.1007/s10549-020-05927-5.
Tang ZR, Zhang R, Lian ZX, Deng SL, Yu K. Estrogen-receptor expression and function in female reproductive disease. Cells. 2019; 8(10):1123. https://doi.org/10.3390/cells8101123.
Kim JH, Choi YK, Byun JK, Kim MK, Kang YN, Kim SH, et al. Estrogen-related receptor γ is upregulated in liver cancer and its inhibition suppresses liver cancer cell proliferation via induction of p21 and p27. EMM. 2016; 48(3): e213-. https://doi.org/10.1038/emm.2015.11
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Hanan H. Hassan, Perry H. Saif ullah

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

















 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


