Bronchiectasis: Etiology, Diagnostic Modalities, and Surgical Management
DOI:
https://doi.org/10.32007/jfacmedbaghdad2505Keywords:
Bronchiectasis; Hemoptysis, Lobectomy; Pulmonary resection; , Video-assisted thoracoscopic surgery (VATS).Abstract
Background: Bronchiectasis is a chronic disease characterized mainly by chronic cough with the production of purulent sputum. It is still seen in Iraq and developing countries, although its incidence is much lower in the developed countries.
Objectives: To highlight the etiology and the diagnostic workup of patients affected by this disease process and to assess the outcome of the surgical intervention in a properly selected patient.
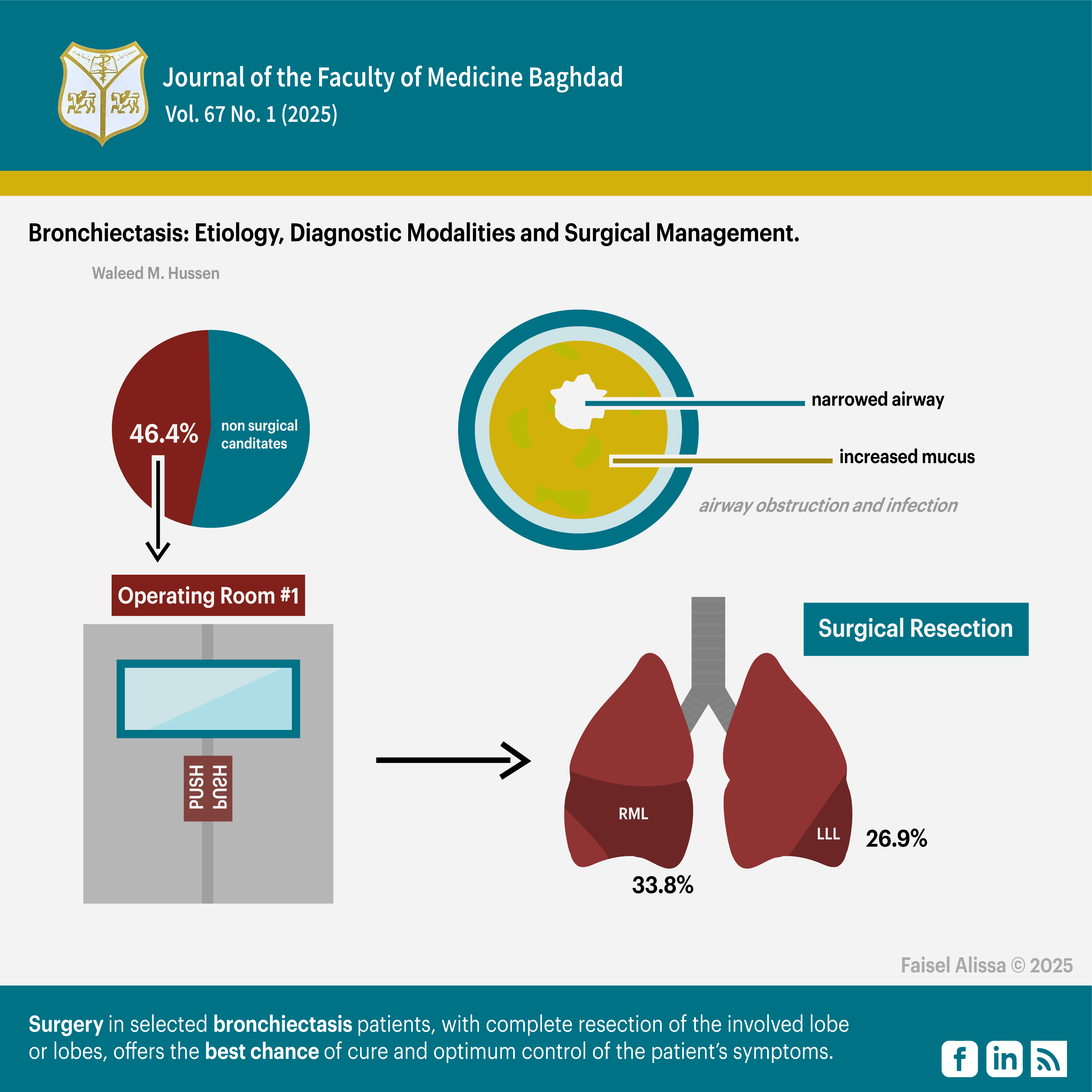
Methods: Fifty-six patients were enrolled in the current study. Thirty patients were excluded as they were not surgical candidates. Twenty-six patients met our criteria, as they were surgical candidates, whose files were studied retrospectively. All the cases were admitted to the Thoracic and Vascular Department of the Surgical Specialties Hospital of the Medical City Teaching Complex, Baghdad/ Iraq, from 1st January 2018 to 31st December 2022. All cases underwent pre-operative blood investigations, diagnostic imaging, and bronchoscopy. They were subjected to surgeries with different resection procedures.
Results: Twenty of the cases were females (76.9%). while six patients were male (23.1%). The youngest patient was a seven-year-old female and the oldest was a 59-year-old male. The mean age was 27.3 years, and the median was 33 years. The most common symptoms were cough with purulent sputum. A CT scan of the chest was performed on all patients. The right middle lobe and the left lower lobe were the most affected. Twenty-five patients underwent classical postero-lateral thoracotomy. The right middle lobe and the left lower lobe were the most common lobes resected. Only one patient underwent video-assisted thoracoscopic surgery (VATS). The histopathological results were consistent with bronchiectasis in 24 patients. Post-operative morbidity included atelectasis and wound infection in one patient, they were managed successfully medically. No mortality was reported in the study.
Conclusion: Once bronchiectasis is well-established, surgery in properly selected patients, with complete resection of the involved lobe or lobes, offers the best chance of cure and optimum control of the patient’s symptoms.
Received: Oct. 2024
Revised: Dec. 2024
Accepted: Dec. 2024
Published April .2025
Downloads
References
. Hill AT, Sullivan AL, Chalmers JD, De Soyza A, Elborn JS, Floto RA, et al. British Thoracic Society Guideline for bronchiectasis in adults. Thorax. 2019 Jan 1;74(Suppl 1):1-69. https://doi.org/10.1136/thoraxjnl-2018-212463
2. Hussain WM, Sultan KM, Momjian RB, Hamdani ZA. Focus on bronchiectasis; Iraqi Postgraduate Medical Journal. 2003, Vol. (2) No. (4)P (388_393). https://www.researchgate.net/publication/358884712_focus_on_Bronchiectasis
3. Aydoğdu K, Çetin M, Yılmaz E, Demiröz ŞM, Türk İ, İncekara F, et al. Analysis of bronchiectasis patients who underwent video-assisted thoracoscopic surgery in a tertiary thoracic surgery center: Ten years of experience. Turkish Journal of Thoracic and Cardiovascular Surgery. 2024 Apr;32(2):202. https://doi.org/10.5606/tgkdc.dergisi.2024.25891
4. Ceylan KC, Batihan G, Kaya ŞÖ, Usluer O, Gürsoy S. Video-assisted thoracic surgery for patients with bronchiectasis: European Respiratory Journal 2020 56: 1721;
https://erj.ersjournals.com/content/56/suppl_64/1721
5. Ocakcioglu I. Uniportal thoracoscopic treatment in bronchiectasis patients: Preliminary experience. Videosurgery and Other Miniinvasive Techniques. 2019; 14(2):304-310
https://doi.org/10.5114/wiitm.2018.78971
6. Hao X, Dazhong L, Lei Y, Jiaying Z, Linyou Z. Surgical treatment of bronchiectasis: 5 years of experience at a single institution. Journal of Laparoendoscopic & Advanced Surgical Techniques. Part A. 2019; 29(6):826-830 https://doi.org/10.1089/lap.2018.0694
7. Choi H, Yang B, Kim YJ, Sin S, Jo YS, Kim Y, et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci Rep. 2021;11:7126. https://doi.org/10.1038/s41598-021-86407-8 8. Vidaillac C, Yong VFL, Jaggi TK, Soh M, Chotirmall SH: Gender differences in bronchiectasis: a real issue? Breathe (Sheff). 2018 Jun; 14(2): 108-121 https://doi.org/10.1183/20734735.000218
9. Wu FJ, Qi Q, Hu Q, [Correlation between chest CT features and clinical characteristics of patients with bronchiectasis]. Zhonghua Yi Xue Za Zhi 2019; 99: 2982-2988. https://pubmed.ncbi.nlm.nih.gov/31607029 / 10. Juergen Biedere. MR imaging of the airways. Br J Radiol Vol .96(1146); 2023 Jun maging of the airways. Br J Radiol Vol .96(1146); 2023 Jun 1 https://doi.org/10.1259/bjr.20220630 11- Adam Nowiński , Katarzyna Stachyra , Maria Szybińska, Michał Bednarek , Robert Pływaczewski Paweł Śliwiński The influence of comorbidities on mortality in bronchiectasis: a prospective, observational study. Adv Clin Exp Med. 2021;30:1315–21. https://doi.org/10.17219/acem/144200
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Waleed M. Hussen, Sabah N. Jaber , Nabeel H. Mohammed

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


