Comparative Adhesion of Pseudomonas aeruginosa to Human Oral Mucosal Epithelial Cells and Polystyrene Surfaces
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632328Keywords:
Adhesion, Antibiotic susceptibility, Biofilm formation, Human oral mucosal epithelial cells, Pseudomonas aeruginosaAbstract
Background: The adhesion of bacteria to biotic and abiotic surfaces reflects their ability to cause infectious diseases. The distinction between the ability of Pseudomonas aeruginosa bacteria to adhere to biotic and abiotic surfaces is not clear in the literature.
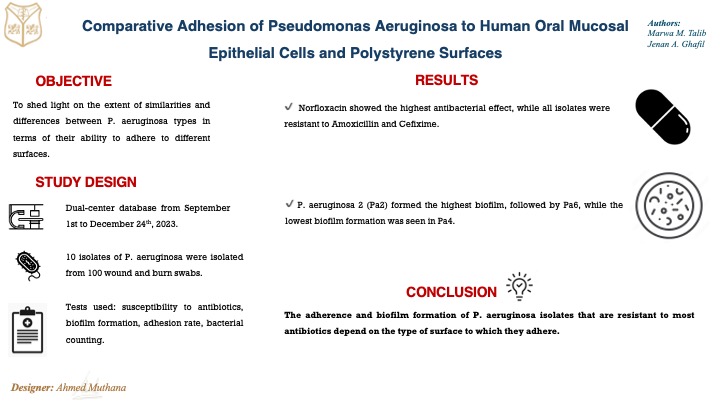
Objectives: The current study aims to shed light on the extent of similarities and differences between P. aeruginosa in terms of their ability to adhere to different biotic and abiotic surfaces.
Materials and Methods: ten isolates of P. aeruginosa were isolated from 100 wound and burn swabs. The isolates were identified using biochemical and phenotypic tests in addition to VITIK-II technology. The susceptibility to antibiotics was estimated using the disc diffusion method. The microtiter-spectrophotometric was used to measure the biofilm formation on polystyrene microtiter plates. The Human oral mucosal epithelial (OMECs) were used to evaluate the adhesion of P. aeruginosa isolates. Plate count and direct bacterial count were used to count the adhered bacteria to human OMECs in vitro.
Results: Norfloxacin showed the highest antibacterial effect while the lowest antibacterial effect was seen in the case of using when Amoxicillin and Cefixime (all isolates were resistant). All isolates from, Pa2 form the highest biofilm followed by Pa6, while the lowest biofilm formation was seen in the case of Pa4. While Pa 6 showed the highest ability to attach to human OMECs followed by Pa2.
Conclusion: It can be concluded that P. aeruginosa isolates are resistant to most antibiotics and that their ability to adhere and biofilm formation depends on the type of surface.
Received: Feb. 2024
Revised: May 2024
Accepted: Jun. 2024
Downloads
References
Rhee C, Kadri SS, Dekker JP, Danner RL, Chen HC, Fram D, et al. CDC Prevention Epicenters Program. Prevalence of Antibiotic-Resistant Pathogens in Culture-Proven Sepsis and Outcomes Associated With Inadequate and Broad-Spectrum Empiric Antibiotic Use. JAMA Netw Open. 2020 3(4):e202899. https://doi.org/10.1001/jamanetworkopen.2020.2899. PMID: 32297949; PMCID: PMC7163409.
Mekonnen H, Seid A, Molla Fenta G, Gebrecherkos T. Antimicrobial resistance profiles and associated factors of Acinetobacter and Pseudomonas aeruginosa nosocomial infection among patients admitted at Dessie comprehensive specialized Hospital, North-East Ethiopia. A cross-sectional study. PLoS One. 2021;16(11):e0257272. https://doi.org/10.1371/journal.pone.0257272P. MID: 34780494; PMCID: PMC8592406.
Kaszab E, Radó J, Kriszt B, Pászti J, Lesinszki V, Szabó A, et al. Groundwater, soil and compost, as possible sources of virulent and antibiotic-resistant Pseudomonas aeruginosa. Int J Environ Health Res. 2021;31(7):848-860. https://doi.org/10.1080/09603123.2019.1691719. Epub 2019 Nov 18. PMID: 31736330.
Ali MN, Zgair AK. Extracellular product of Pseudomonas aeruginosa in growth medium is involved in the pro-inflammatory cytokine response of human oral epithelial cells in vitro. Polim Med. 2022; 52(2):77-82. https://doi.org/10.17219/pim/155849. PMID: 36449403.
Groeger S, Meyle J. Oral Mucosal Epithelial Cells. Front Immunol. 2019; 10:208 https://doi.org/10.3389/fimmu.2019.00208. PMID: 30837987; PMCID: PMC6383680.
Laventie, B.-J. and U. Jenal, Surface sensing and adaptation in bacteria. Annual review of microbiology. 2020; 74: 735-760. https://doi.org/10.1146/annurev-micro-012120-0634277
Chhibber S, Zgair AK. Adhesion of Stenotrophomonas maltophilia to Biotic and Abiotic Surfaces and Role of Flagella in Bacterial Adhesion. World J Exp Biosci. 2022; 10(2), 26-31
https://www.bing.com/ck/a?!&&p=ecf3 .
Ou-yahia D, Fikri-Benbrahim K, Bennouna F, Koraichi SI. Adhesion of Pseudomonas aeruginosa and its effects on the physicochemical properties of 304 stainless steel immersed in artificial seawater. Materials Today: Proceedings. 2023;72, 3589-3593. https://doi.org/10.1016/j.surfin.2018.04.004.
Etha SA, Sivasankar VS, Sachar HS, Das S. Coating for preventing nonspecific adhesion mediated biofouling in salty systems: Effect of the electrostatic and van der waals interactions. Electrophoresis. 2020;41(9):657-665. https://doi.org10.1002/elps.201900348. Epub 2020 Mar 12. PMID: 32092163.
Mohammed AJ, Kanber SA, Talib MM, Rasheed HJ. Bioremediation of crude oil pollutants in the soil by Pseudomonas aeruginosa and other soil microorganisms.World J Exp Biosci11. 2023; (1): 07-10. URL
Ali M A, Mahmood SS. Role of Rnd-efflux pump in levofloxacin resistance among Acinetobacter baumannii. Iraqi J Agricul Sci. 2022; 53(3), pp. 542–550. https://doi.org/10.36103/ijas.v53i3.1562.
Salman AD, Amer Z, Abud_Rahman ES. Bacteriological study of Pseudomonas aeruginosa isolated from different infections and study antimicrobial activities of plant extract Solanum Nigrum against it. Iraqi J Sci. 2017; 58 (4C):2278-84.https://doi.org/10.24996/ijs.2017.58.4C.
Hsueh PR, Ko WC, Wu JJ, Lu JJ, Wang FD, et al. Consensus statement on the adherence to Clinical and Laboratory Standards Institute (CLSI) Antimicrobial Susceptibility Testing Guidelines (CLSI-2010 and CLSI-2010-update) for Enterobacteriaceae in clinical microbiology laboratories in Taiwan. J Microbiol Immunol Infect. 2010; 43(5):452-5. https://doi.org/10.1016/S1684-1182(10)60070-9.
Al-Mutalib LAA, Zgair AK. Effect of subinhibitory doses of rifaximin on in vitro Pseudomonas aeruginosa adherence and biofilm formation to biotic and abiotic surface models. Polim Med. 2023; 53(2):97-103. https://doi.org/10.17219/pim/166584. PMID: 37470308.
Yang Y, Schwiderek S, Grundmeier G, Keller A. Strain-Dependent Adsorption of Pseudomonas aeruginosa-Derived Adhesin-Like Peptides at Abiotic Surfaces. Micro 2021;1, 129–139. https://doi.org/10.3390/micro1010010.
Muggeo A, Coraux C, Guillard T. Current concepts on Pseudomonas aeruginosa interaction with human airway epithelium. PLoS Pathog. 2023 ;19(3):e1011221.https://doi.org/10.1371/journal.ppat.1011221. PMID: 36996043; PMCID: PMC10062669.
Huang P, Li Z, Liu R, Bartlam M, Wang Y. Polystyrene nanoparticles induce biofilm formation in Pseudomonas aeruginosa. J Hazard Mater. 2024;469:133950.https://doi.org/10.1016/j.jhazmat.2024.133950. Epub 2024. PMID: 38442601.
Geiger CJ, O'Toole GA. Evidence for the Type IV Pilus Retraction Motor PilT as a Component of the Surface Sensing System in Pseudomonas aeruginosa. J Bacteriol. 2023; 205(7):e0017923. https://doi.org/10.1128/jb.00179-23.
Thi MTT, Wibowo D, Rehm BHA. Pseudomonas aeruginosa Biofilms. Int. J. Mol. Sci. 2020, 21, 8671. https://doi.org/10.3390/ijms21228671
Kreve S, Reis ACD. Bacterial adhesion to biomaterials: What regulates this attachment? A review. Jpn Dent Sci Rev. 2021 Nov;57:85-96. https://doi.org/10.1016/j.jdsr.2021.05.003. Epub 2021 Jun 12. PMID: 34188729; PMCID: PMC8215285.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Marwa M. Talib, Jenan A. Ghafil

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


