Study of ATPase and GTPase levels in Fibrotic Lung Disease with and without COVID-19 Vaccination
DOI:
https://doi.org/10.32007/jfacmedbagdad.6622272Keywords:
ATPase;, GTPase;, , COVID-19 Vaccination; , Fibrotic Lung Disease.Abstract
Background: In eukaryotic cells, the acidification of intracellular compartments is the responsibility of vacuolar H+ ATPase, a family of proton pumps, sometimes known as V-ATPases. Small GTPases are signaling molecules that regulate important cellular processes as well as subcellular activities making them essential players, particularly in a wide variety of coronavirus infection processes.
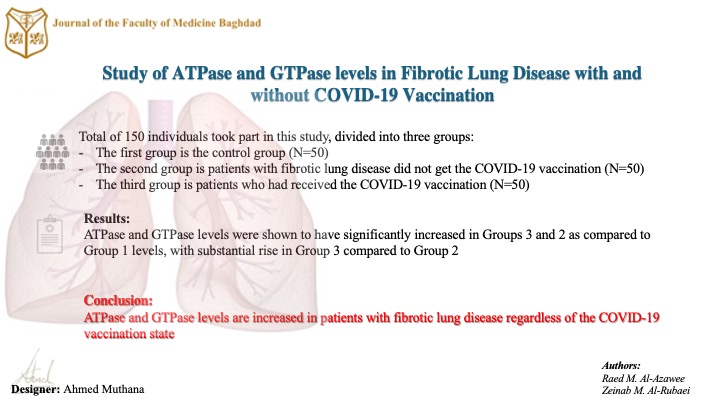
Objectives: The purpose of this research was to assess the levels of ATPase and GTPase in fibrotic lung disease patients who had received or had not received the COVID-19 vaccination, and then to compare these levels with those of the control group.
Methods: A total of 150 individuals participated in this study, divided into three groups. The first group was the control group (N=50). In the second group (N=50) patients with fibrotic lung disease () who did not get the COVID-19 vaccination. Fifty patients who had received the COVID-19 vaccination made up the third group ()(N=50). Enzyme-linked immunosorbent assay was the method that was used to determine the amounts of ATPase and GTPase. The P- P-value of 0.05 or less is considered statistically significant. ROC tests were examined for ATPase and GTPase.
Results: The data analysis reported a significant rise in alkaline phosphatase, Alanine aminotransferase, and Aspartate-aminotransferase () among the three groups. Both ATPase and GTPase levels were shown to have significantly increased in Groups 3 and 2 as compared to Group 1 levels. Moreover, a substantial rise was discovered in Group 3 in comparison to Group 2 which was detected.
Conclusion: ATPase and GTPase levels are increased in patients with fibrotic lung disease regardless of the COVID-19 vaccination state.
Received: Dec. 2023
Revised: Mar, 2024
Accepted: April. 2024
Downloads
References
- Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, eta al . Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. American journal of respiratory and critical care medicine. 2018 Sep 1;198(5):e44-68. https://doi.org/10.1164/rccm.201807-1255st.
- Auda IG, Auda J, Salih RH. SARS-CoV-2 and other Coronaviruses: A matter of variations. Al-Kindy College Medical Journal. 2023 Apr 30;19(1):5-10. https://doi.org/10.47723/kcmj.v19i1.927 .
- Jasim RZ. Biochemical Action of Vaccines in Iraqi Patients with COVID-19 Infection. Baghdad Science Journal. 2023 Aug 30;20(4 (SI)):1469-79. https://dx.doi.org/10.21123/bsj.2023.8750.
- Solomon JJ, Heyman B, Ko JP, Condos R, Lynch DA. CT of post-acute lung complications of COVID-19. Radiology. 2021 Nov;301(2):E383-95. https://doi.org/10.1148/radiol.2021211396.
- Wong AW, Fidler L, Marcoux V, Johannson KA, Assayag D, Fisher JH, et al. Practical considerations for the diagnosis and treatment of fibrotic interstitial lung disease during the coronavirus disease 2019 pandemic. Chest. 2020 Sep 1;158(3):1069-78. https://doi.org/10.1016%2Fj.chest.2020.04.019.
- Park MS, Kim JI, Lee I, Park S, Bae JY, Park MS. Towards the application of human defensins as antivirals. Biomolecules & therapeutics. 2018 May;26(3):242. https://doi.org/10.4062/biomolther.2017.172.
- Lee JU, Hong J, Shin H, Ryu CB, Park SW, Jeong SH. Overexpression of V-ATPase B2 attenuates lung injury/fibrosis by stabilizing lysosomal membrane permeabilization and increasing collagen degradation. Experimental & Molecular Medicine. 2022 May;54(5):662-72. https://doi.org/10.1038/s12276-022-00776-2 .
- Li X, Villacreses R, Thornell IM, Noriega J, Mather S, Brommel CM, et al . V-type ATPase mediates airway surface liquid acidification in pig small airway epithelial cells. American journal of respiratory cell and molecular biology. 2021 Aug;65(2):146-56. https://doi.org/10.1165/rcmb.2020-0349oc.
- Shimokawa H, Sunamura S, Satoh K. RhoA/Rho-kinase in the cardiovascular system. Circulation research. 2016 Jan 22;118(2):352-66. https://doi.org/10.1161/circresaha.115.306532 .
- Yoshii A, Iizuka K, Dobashi K, Horie T, Harada T, Nakazawa T, et al . Relaxation of contracted rabbit tracheal and human bronchial smooth muscle by Y-27632 through inhibition of Ca2+ sensitization. American Journal of Respiratory Cell and Molecular Biology. 1999 Jun 1;20(6):1190-200. https://doi.org/10.1165/ajrcmb.20.6.3441 .
- Nagpal P, Guo J, Shin KM, Lim JK, Kim KB, Comellas AP, et al. Quantitative CT imaging and advanced visualization methods: potential application in novel coronavirus disease 2019 (COVID-19) pneumonia. BJR| Open. 2021 Feb;3(1):20200043. https://doi.org/10.1259/bjro.20200043 .
- Al-Mendalawi MD. Two Decades in the Journey of Al-Kindy College Medical Journal: Key Barriers, Achievements, and Prospects. Al-Kindy College Medical Journal. 2022 May 8;18(1):3-4. https://doi.org/10.47723/kcmj.v18i1.838 .
- Al-Hamamy HR. The impact of COVID-19 on healthy related issues, a structured review. Al-Kindy College Medical Journal. 2021 Dec 30;17(3):152-7. https://doi.org/10.47723/kcmj.v17i3.419.
- Lami F, Elfadul M, Rashak H, Al Nsour M, Akhtar H, Khader Y, et al. Risk factors of COVID-19 critical outcomes in the Eastern Mediterranean Region: multicountry retrospective study. JMIR Public Health and Surveillance. 2022 Mar 15;8(3):e32831. https://doi.org/10.2196/32831
- Faraj AM, Qadir SA, Mohammed OA, Aziz PY, Alkhafaji M, Rahman HS, et al. Current potential options for COVID-19 treatment in Iraq-Kurdistan region and the rest of the world: A mini-review. Iraqi Journal of Science. 2022 Mar 30:948-58. https://doi.org/10.24996/ijs.2022.63.3.4 .
- Hamid MK. Impact of COVID-19 Vaccine on Hearing Status of Young Ages (Medical College Students as a Sample). Baghdad Science Journal. 2023 Aug 30;20(4 (SI)):1498-. https://doi.org/10.21123/bsj.2023.8694
- Mustafa MW. Audio logical profile of asymptomatic Covid-19 PCR-positive cases. American journal of otolaryngology. 2020 May 1;41(3):102483. https://doi.org/10.1016/j.amjoto.2020.102483.
- Mohammad AM, Attia H, Ali YH. Comparative Analysis of MFO, GWO and GSO for Classification of Covid-19 Chest X-Ray Images. Baghdad Science Journal. 2023 Aug 30;20(4 (SI)):1540-. http://dx.doi.org/10.21123/bsj.2023.9236.
- Sulayman N. Deep Learning-based Predictive Model of mRNA Vaccine Deterioration: An Analysis of the Stanford COVID-19 mRNA Vaccine Dataset. Baghdad Science Journal. 2023 Aug 30;20(4 (SI)):1451-8. https://doi.org/10.21123/bsj.2023.8504.
- Kavsak PA, de Wit K, Worster A. Emerging key laboratory tests for patients with COVID-19. Clinical biochemistry. 2020 Jul;81:13. https://doi.org/10.1016%2Fj.clinbiochem.2020.04.009.
- Samsudin I, Vasikaran SD. Clinical utility and measurement of procalcitonin. The Clinical Biochemist Reviews. 2017 Apr;38(2):59. https://pubmed.ncbi.nlm.nih.gov/29332972.
- Salman ZZ, Mohammed SB, Muhi SA. Studying the Effect of COVID-19 on Liver Enzymes and Lipid Profile in Iraqi Recovering Patients. Baghdad Science Journal. 2023 Aug 30;20(4 (SI)):1489-. https://doi.org/10.21123/bsj.2023.8347.
- Baroiu L, Dumitru C, Iancu A, Leșe AC, Drăgănescu M, Baroiu N, Anghel L. COVID-19 impact on the liver. World Journal of Clinical Cases. 2021 Jun 6;9(16):3814. https://doi.org/10.12998%2Fwjcc.v9.i16.3814.
- Chai X, Hu L, Zhang Y, Han W, Lu Z, Ke A, et al. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. biorxiv. 2020 Feb 4:2020-02. https://doi.org/10.1101/2020.02.03.931766
- Lin CW, Tsai FJ, Wan L, Lai CC, Lin KH, Hsieh TH, et al. Binding interaction of SARS coronavirus 3CLpro protease with vacuolar-H+ ATPase G1 subunit. FEBS letters. 2005 Nov 7;579(27):6089-94. https://doi.org/10.1016%2Fj.febslet.2005.09.075.
- Wang R, Wang J, Hassan A, Lee CH, Xie XS, Li X. Molecular basis of V-ATPase inhibition by bafilomycin A1. Nature communications. 2021 Mar 19;12(1):1782. https://doi.org/10.1038/s41467-021-22111-5.
- Li X, Villacreses R, Thornell IM, Noriega J, Mather S, Brommel CM, et al. V-type ATPase mediates airway surface liquid acidification in pig small airway epithelial cells. American journal of respiratory cell and molecular biology. 2021 Aug;65(2):146-56. https://doi.org/10.1165/rcmb.2020-0349oc
- Biancatelli RM, Solopov PA, Sharlow ER, Lazo JS, Marik PE, Catravas JD. The Pathophysiology of COVID-19 and SARS-CoV-2 Infection: The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2021 Aug 8;321(2):L477. https://doi.org/10.1152/ajplung.00223.2021 .
- Lv X, Li Z, Guan J, Hu S, Zhang J, Lan Y, et al. Porcine hem agglutinating encephalomyelitis virus activation of the integrin α5β1-FAK-cofilin pathway causes cytoskeletal rearrangement to promote its invasion of N2a cells. Journal of virology. 2019 Mar 1;93(5):10-128. https://doi.org/10.1128%2FJVI.01736-18.
- Li Z, Zhao K, Lan Y, Lv X, Hu S, Guan J, et al. Porcine hem agglutinating encephalomyelitis virus enters neuro-2a cells via clathrin-mediated endocytosis in a Rab5-, cholesterol-, and pH-dependent manner. Journal of virology. 2017 Dec 1;91(23):10-128. https://doi.org/10.1128%2FJVI.01083-17.
- Mattioli B, Straface E, Matarrese P, Quaranta MG, Giordani L, Malorni W, et al. Leptin as an immunological adjuvant: enhanced migratory and CD8+ T cell stimulatory capacity of human dendritic cells exposed to leptin. The FASEB Journal. 2008 Jun;22(6):2012-22. https://doi.org/10.1096/fj.07-098095.
- Zhang S, Kazanietz MG, Cooke M. Rho GTPases and the emerging role of tunneling nanotubes in physiology and disease. American Journal of Physiology-Cell Physiology. 2020 Nov 1;319(5):C877-84. https://doi.org/10.1152%2Fajpcell.00351.2020
- Hou W, Wang S, Wu H, Xue L, Wang B, Wang S, et al. Small GTPase—A Key Role in Host Cell for Coronavirus Infection and a Potential Target for Coronavirus Vaccine Adjuvant Discovery. Viruses. 2022 Sep 14;14(9):2044. https://doi.org/10.3390/v14092044
- Segatori VI, Garona J, Caligiuri LG, Bizzotto J, Lavignolle R, Toro A, et al. Effect of ivermectin and atorvastatin on nuclear localization of importin alpha and drug target expression profiling in host cells from nasopharyngeal swabs of SARS-CoV-2-positive patients. Viruses. 2021 Oct 15;13(10):2084. https://doi.org/10.3390/v13102084.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Raed M. Al-Azawee, Zeinab M. Al-Rubaei

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


