The Role of Kisspeptin in Intracytoplasmic Sperm Injection Cycles in a Group of Infertile Iraqi Females
DOI:
https://doi.org/10.32007/jfacmedbaghdad3032الكلمات المفتاحية:
Kisspeptin، Follicular Fluid، Fertilization، Oocytes، Ovarian Follicleالملخص
Background: Infertility is a global issue that not only affects individuals but also impacts society as a whole. Kisspeptin has emerged as a key player in the understanding of certain facets of infertility. However, research on the role of kisspeptin in fertility, particularly in assisted reproductive treatment, remains limited.
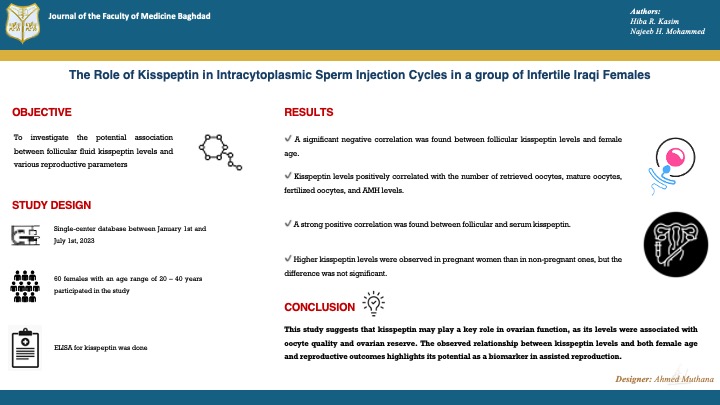
Objectives: To investigate the potential association between follicular fluid kisspeptin levels and various reproductive parameters, including the number and maturity of oocytes, fertilization rate, pregnancy detection, anti-Müllerian hormone levels, and the age of females.
Methods: Sixty infertile couples with an age range of 20 – 40 years participated in this study. They complained of unexplained infertility, had no hormonal or male factors, all with the same stimulation protocol, with follicular fluid collected on the day the oocytes were retrieved. These follicular fluid samples were centrifuged and then frozen at -20ºC until the day an enzyme-linked immunosorbent assay (ELISA) for kisspeptin was done. The study was conducted at the High Institute for Infertility Diagnosis and Assisted Reproductive Technology, Al-Nahrain University, Baghdad, between the 1st of January to the 1st of July, 2023.
Results: A significant negative correlation was found between follicular kisspeptin levels and female age. Kisspeptin levels positively correlated with the number of retrieved oocytes, mature oocytes, fertilized oocytes, and AMH levels. Higher kisspeptin levels were observed in pregnant women (707.7 ± 235.28 pg/mL) than in non-pregnant ones (648.9 ± 215.27 pg/mL), but the difference was not significant. A strong positive correlation was found between follicular and serum kisspeptin.
Conclusion: This study suggested that kisspeptin may play a key role in ovarian function, as its levels were associated with oocyte quality and ovarian reserve. The observed relationship between kisspeptin levels and both female age and reproductive outcomes highlights its potential as a biomarker in assisted reproduction.
المراجع
1. Qin L, Sitticharoon C, Petyim S, Keadkraichaiwat I, Sririwichitchai R, Maikeaw P, et al. Roles of kisspeptin in IVF/ICSI-treated infertile women and in human granulosa cells. Exp Biol Med. 2021;246(8):996-1010. https://doi.org/10.1177/1535370220981006. DOI: https://doi.org/10.1177/1535370220981006
2. Haddad NIA, Hussein EA, Hassan IT. A prospective study: Correlation between serum estradiol levels and fertilization rates in assisted reproductive technology outcomes. J Biosci Appl Res. 2024;10(1):77-84. https://doi.org/10.21608/jbaar.2024.348043. DOI: https://doi.org/10.21608/jbaar.2024.348043
3. Shakir RA, Badr AH, Jassim NA, Hummadi JA. Prevalence of fibromyalgia in infertile women. J Fac Med Baghdad. 2019 May 12;60(4):228-33. https://doi.org/10.32007/jfacmedbagdad.604700. DOI: https://doi.org/10.32007/jfacmedbagdad.604700
4. Yun S, Kim DK, Furlong M, Hwang JI, Vaudry H, Seong JY. Does kisspeptin belong to the proposed RF-amide peptide family? Front Endocrinol (Lausanne). 2014;5(AUG):22-6. https://doi.org/10.3389/fendo.2014.00134. DOI: https://doi.org/10.3389/fendo.2014.00134
5. Mumtaz A, Khalid A, Jamil Z, Fatima SS, Arif S, Rehman R. Kisspeptin: A potential factor for unexplained infertility and impaired embryo implantation. Int J Fertil Steril. 2017;11(2):99-104. https://doi.org/10.22074/ijfs.2017.4957.
6. Bowe JE, Hill TG, Hunt KF, Smith LIF, Simpson SJS, Amiel SA, et al. A role for placental kisspeptin in β cell adaptation to pregnancy. JCI Insight. 2019;4(20). https://doi.org/10.1172/jci.insight.124540. DOI: https://doi.org/10.1172/jci.insight.124540
7. Chakravarthi VP, Khristi V, Ghosh S, Yerrathota S, Dai E, Roby KF, et al. ESR2 is essential for gonadotropin-induced Kiss1 expression in granulosa cells. Endocrinology. 2018;159(11):3860-73. https://doi.org/10.1210/en.2018-00608. DOI: https://doi.org/10.1210/en.2018-00608
8. Harter CJL, Kavanagh GS, Smith JT. The role of kisspeptin neurons in reproduction and metabolism. J Endocrinol. 2018;238(3):R173-83. https://doi.org/10.1530/JOE-18-0108. DOI: https://doi.org/10.1530/JOE-18-0108
9. Hu KL, Chang HM, Zhao HC, Yu Y, Li R, Qiao J. Potential roles for the kisspeptin/kisspeptin receptor system in implantation and placentation. Hum Reprod Update. 2019;25(3):326-43. https://doi.org/10.1093/humupd/dmy046. DOI: https://doi.org/10.1093/humupd/dmy046
10. Sun P, Zhang Y, Sun L, Sun N, Wang J, Ma H. Kisspeptin regulates the proliferation and apoptosis of ovary granulosa cells in polycystic ovary syndrome by modulating the PI3K/AKT/ERK signaling pathway. BMC Womens Health . 2023;23(1):1-11.
https://doi.org/10.1186/s12905-022-02154-6. DOI: https://doi.org/10.1186/s12905-022-02154-6
11. Guzman S, Dragan M, Kwon H, de Oliveira V, Rao S, Bhatt V, et al. Targeting hepatic kisspeptin receptor ameliorates nonalcoholic fatty liver disease in a mouse model. J Clin Invest. 2022;132(10):1-19. https://doi.org/10.1172/JCI145889. DOI: https://doi.org/10.1172/JCI145889
12. Alawad ZM. Level of follicular fluid vitamin D and embryo quality in a sample of Iraqi women undergoing IVF. J Fac Med Baghdad. 2019 May 12;60(4):215-21. https://doi.org/10.32007/jfacmedbagdad.604758 DOI: https://doi.org/10.32007/jfacmedbagdad.604758
13. Taniguchi Y, Kuwahara A, Tachibana A, Yano Y, Yano K, Yamamoto Y, et al. Intra-follicular kisspeptin levels are related to oocyte maturation and gonadal hormones in patients who are undergoing assisted reproductive technology. Reprod Med Biol. 2017;16(4):380-5. https://doi.org/10.1002/rmb2.12056. DOI: https://doi.org/10.1002/rmb2.12056
14. Ruohonen ST, Gaytan F, Usseglio Gaudi A, Velasco I, Kukoricza K, Perdices-Lopez C, et al. Selective loss of kisspeptin signaling in oocytes causes progressive premature ovulatory failure. Hum Reprod. 2022;37(4):806-21. https://doi.org/10.1093/humrep/deab287. DOI: https://doi.org/10.1093/humrep/deab287
15. Al Najar AF. Prevalence and pattern of endocrinological abnormalities in oligospermic and azoospermic patients. J Fac Med Baghdad. 2011 Jan 2;52(4):402-4. https://doi.org/10.32007/jfacmedbagdad.524941. DOI: https://doi.org/10.32007/jfacmedbagdad.524941
16. Byri P, Gangineni A, Reddy KR, Raghavender KBP. Effect of kisspeptin on in vitro maturation of sheep oocytes. Vet World. 2017;10(3):276-80. https://doi.org/10.14202/vetworld.2017.276-280. DOI: https://doi.org/10.14202/vetworld.2017.276-280
17. Trevisan CM, Montagna E, De Oliveira R, Christofolini DM, Barbosa CP, Crandall KA, et al. Kisspeptin/GPR54 system: What do we know about its role in human reproduction? Cell Physiol Biochem. 2018;49(4):1259-76. https://doi.org/10.1159/000493406. DOI: https://doi.org/10.1159/000493406
18. Zahid ZR. Creating genetic system. J Fac Med Baghdad. 2012 Jul 1;54(2):115-7. https://doi.org/10.32007/jfacmedbagdad.542737 DOI: https://doi.org/10.32007/jfacmedbagdad.542737
19. Yu H, Liu J, Guo H, Chen C, Han Y, Cui Y. Prognostic value of repeated serum kisspeptin measurements in early first trimester pregnancy: A preliminary study. Reprod Biomed Online [Internet]. 2019;38(3):465-71. https://doi.org/10.1016/j.rbmo.2018.11.014. DOI: https://doi.org/10.1016/j.rbmo.2018.11.014
20. Alanssari SAM, Kjelland JLM, Albananchi MR, Kraemer DC. In vitro fertilization of immature oocytes by testicular sperm: Animal model for azoospermic infertile patients. J Fac Med Baghdad. 2008 Jan 2 [cited 2024 Aug 13];49(4):394-9. https://doi.org/10.32007/jfacmedbagdad.4941329. DOI: https://doi.org/10.32007/jfacmedbagdad.4941329
21. Xin X, Li Z, Zhong Y, Li Q, Wang J, Zhang H, et al. KISS1 suppresses apoptosis and stimulates the synthesis of E2 in porcine ovarian granulosa cells. Animals. 2019;9(2). https://doi.org/10.3390/ani9020054. DOI: https://doi.org/10.3390/ani9020054
22. Sudek HL. Ovarian antral follicle number and the amount of gonadotropin used in ovarian stimulation in polycystic ovarian patients. J Fac Med Baghdad. 2011 Jul 3;53(2):228-32. https://doi.org/10.32007/jfacmedbagdad.532880
23. Owens LA, Abbara A, Lerner A, O'floinn S, Christopoulos G, Khanjani S, et al. The direct and indirect effects of kisspeptin-54 on granulosa lutein cell function. Hum Reprod. 2018;33(2):292-302. https://doi.org/10.1093/humrep/dex357. DOI: https://doi.org/10.1093/humrep/dex357
24. Cao Y, Li Z, Jiang W, Ling Y, Kuang H. Reproductive functions of kisspeptin/KISS1R systems in the periphery. Reprod Biol Endocrinol. 2019;17(1):1-9. doi: 10.1186/s12958-019-0511-x. DOI: https://doi.org/10.1186/s12958-019-0511-x
25. Bedenk J, Vrtačnik-Bokal E, Virant-Klun I. The role of anti-Müllerian hormone (AMH) in ovarian disease and infertility. J Assist Reprod Genet. 2020;37(1):89-100. https://doi.org/10.1007/s10815-019-01622-7. DOI: https://doi.org/10.1007/s10815-019-01622-7
26. Hussein EA, Talib Hassan I, Abdulkareem Abu-Ragheef M, Sahib Khalil N, Ali Haddad R. Follicular glypican-1 as a predictive marker of reproductive outcomes in women undergoing IVF/ICSI [Internet]. Systematic Reviews in Pharmacy. 2020;11:1-6. http://www.sysrevpharm.org/.
27. Al-Brazanchi T, Al-Anssari SM, Khunda SS, Allow AK, Kanan ZK. Women age and embryo implantation following intracytoplasmic sperm injection and embryo transfer in infertile patients. J Fac Med Baghdad. 2006 Jul 2;48(2):155-61. https://doi.org/10.32007/jfacmedbagdad.4821528. DOI: https://doi.org/10.32007/jfacmedbagdad.4821528
28. Kasman AM, Zhang CA, Luke B, Eisenberg ML. Association between infertility and mental health of offspring in the United States: A population-based cohort study. Hum Fertil. 2022;25(2):384-9. https://doi.org/10.1080/14647273.2020.1805799. DOI: https://doi.org/10.1080/14647273.2020.1805799
29. Massarotti C, Gentile G, Ferreccio C, Scaruffi P, Remorgida V, Anserini P. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol Endocrinol. 2019;35(6):485-9. https://doi.org/10.1080/09513590.2018.1540575. DOI: https://doi.org/10.1080/09513590.2018.1540575
30. Salman FS, Al-Qadhi H, Al-Kareem B. N-acetyl cysteine's effect on semen parameters in a sample of Iraqi men with oligoasthenoteratozoospermia. J Fac Med Baghdad [Internet]. 2022 Oct 17;64(3):170-4. https://doi.org/10.32007/jfacmedbagdad.6431938. DOI: https://doi.org/10.32007/jfacmedbagdad.6431938
31. Fauser BC. Towards the global coverage of a unified registry of IVF outcomes. Reprod Biomed Online. 2019;38(2):133-7. https://doi.org/10.1016/j.rbmo.2018.12.001. DOI: https://doi.org/10.1016/j.rbmo.2018.12.001
32. Hassan IT, Hussein EA, Abdulkareem M, Ragheef A, Haddad RA, Khalil NS. Follicular and serum testosterone as a predictor of assisted reproductive technology outcomes in infertile polycystic ovarian syndrome patients. 2020;7319(December):7315-9.
33. Findlay JK, Hutt KJ, Hickey M, Anderson RA. How is the number of primordial follicles in the ovarian reserve established? Biol Reprod. 2015;93(5):1-7. https://doi.org/10.1095/biolreprod.115.133652 DOI: https://doi.org/10.1095/biolreprod.115.133652
34. Sudek HL. Ovarian antral follicle number and the amount of gonadotropin used in ovarian patients. J Fac Med Baghdad [Internet]. 2011 Jul 3;53(2):228-32. https://doi.org/10.32007/jfacmedbagdad.532880. DOI: https://doi.org/10.32007/jfacmedbagdad.532880
35. Knox RV. Follicle development in pigs: State of the art. Mol Reprod Dev. 2023;90(7):480-90. https://doi.org/10.1002/mrd.23576. DOI: https://doi.org/10.1002/mrd.23576
36. Ahmed HS, Abbas AK. The relation between reproductive hormones and metabolic parameters in women with polycystic ovary syndrome. J Fac Med Baghdad [Internet]. 2014 Jul 1;56(2):229-33. https://doi.org/10.32007/jfacmedbagdad.562483 DOI: https://doi.org/10.32007/jfacmedbagdad.562483
37. Abbara A, Jayasena CN, Christopoulos G, Narayanaswamy S, Izzi-Engbeaya C, Nijher GMK, et al. Efficacy of kisspeptin-54 to trigger oocyte maturation in women at high risk of ovarian hyperstimulation syndrome (OHSS) during in vitro fertilization (IVF) therapy. J Clin Endocrinol Metab. 2015;100(9):3322-31. https://doi.org/10.1210/jc.2015-2332. DOI: https://doi.org/10.1210/jc.2015-2332
38. Masumi S, Lee EB, Dilower I, Upadhyaya S, Chakravarthi VP, Fields PE, et al. The role of kisspeptin signaling in oocyte maturation. Front Endocrinol (Lausanne). 2022;13(August):1-15. https://doi.org/10.3389/fendo.2022.917464. DOI: https://doi.org/10.3389/fendo.2022.917464
39. Bódis J, Sulyok E, Kőszegi T, Prémusz V, Várnagy Á, Koppán M. Serum and follicular fluid levels of serotonin, kisspeptin, and brain-derived neurotrophic factor in patients undergoing in vitro fertilization: An observational study. J Int Med Res. 2019;48(4):1-9. https://doi.org.1177/0300060519879330. DOI: https://doi.org/10.1177/0300060519879330
40. Rhman R, Zafar A, Ali AA, Baig M, Alam F. Impact of serum and follicular fluid kisspeptin and estradiol on oocyte maturity and endometrial thickness among unexplained infertile females during ICSI. PLoS One. 2020;15(10):e0239142. https://doi.org/10.1371/journal.pone.0239142. DOI: https://doi.org/10.1371/journal.pone.0239142
التنزيلات
منشور
إصدار
القسم
الفئات
الرخصة
الحقوق الفكرية (c) 2025 Hiba R. Qasim, Najeeb H. Mohammed

هذا العمل مرخص بموجب Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


