Assessment of Intestinal Hormones Cholecystokinin and Peptide YY in Iraqi Women with Polycystic Ovarian Syndrome.
DOI:
https://doi.org/10.32007/jfacmedbaghdad2441Keywords:
Cholecystokinin, Follicle-Stimulating Hormone, Luteinizing Hormone, Peptide YY, ProlactinAbstract
Background: Among the most prevalent hormonal, reproductive and metabolic issues impacting women is polycystic ovarian syndrome. Also, insulin resistance raises the chance of developing chronic illnesses in women with polycystic ovarian syndrome, including diabetes mellitus, cardiovascular disease, metabolic syndrome, and potentially endometrial and breast malignancies.
Objectives: Measurement of two intestinal hormones (cholecystokinin, peptide YY), luteinising hormone, follicle-stimulating hormone, and Prolactin. Waist and wrist circumference were measured in centimeters
Methods: A sample of polycystic ovarian syndrome women who were referred to the Medical City of Baghdad hospital for management of their infertility were recruited in the current study. Sixty polycystic ovarian syndrome patients were split into two groups based on Body Mass Index: thirty obese polycystic ovarian syndrome women and thirty overweight polycystic ovarian syndrome women. In addition, thirty healthy control women were added as a third group, whose average age was between 20 and 35 years. Polycystic ovarian syndrome in women was diagnosed using two of the three diagnostic criteria: polycystic ovaries in ultrasound, oligo or anovulation, and hyperandrogenism. The investigation ran from October 2023 until January 2024. The investigations of the patient were requested, and all data in the study were added.
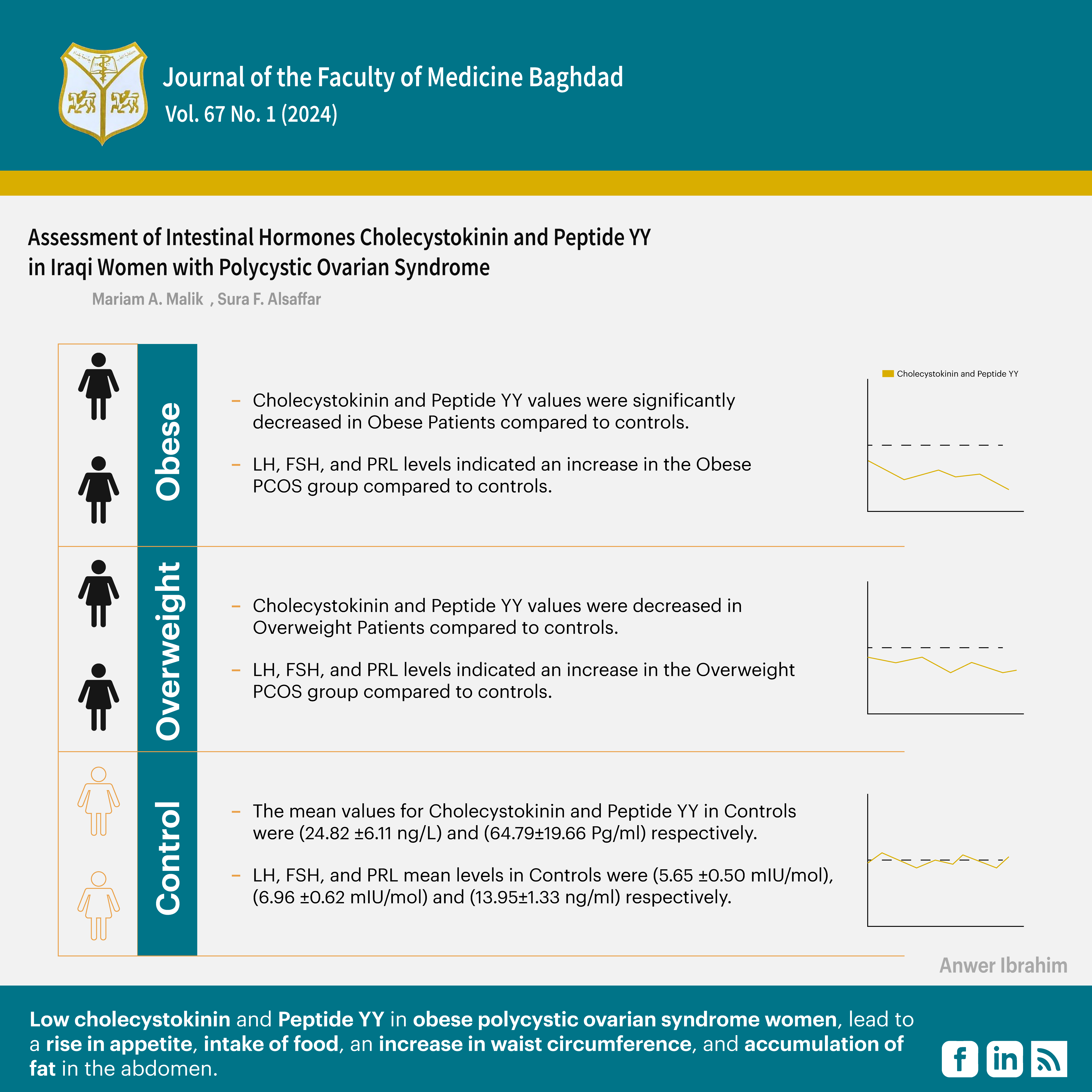
Results: Obese women with polycystic ovarian syndrome had significantly higher levels of waist circumference 102.75 ±1.45, prolactin 20.48 ±1.43, luteinizing hormone 7.85 ±0.56, Follicle-stimulating hormone 8.41 ±0.38, and lower levels of Peptide YY 45.33±16.62, and cholecystokinin 14.37 ±3.64.
Conclusion: Low cholecystokinin and Peptide YY in obese polycystic ovarian syndrome women lead to a rise in appetite, intake of food, an increase in waist circumference, and accumulation of fat in the abdomen.
Received: Aug., 2024
Revised: Nov., 2024
Accepted: Jan. 2025
Published: April 2025
Downloads
References
1. Shenta A, Saud K, Al-Shawi A. Assessment the correlations of hormones, lipid profiles, oxidative stress, and Zinc Concentration in Iraqi Women with Polycystic Ovary Syndrome. Reports of Biochemistry & Molecular Biology. 2020 Oct;9(3):270. https://doi.org/10.29252/rbmb.9.3.270.
2. Nurain AS, Basuki SW, Kurniati YP, Sintowati R. The Relationship Between Obesity and Level of Polycystic Ovary Syndrome (PCOS): Literature Review. In International Conference on Health and Well-Being (ICHWB 2021) 2022; 218-226. https://doi.org10.2991/ahsr.k.220403.030.
3. Rehfeld JF. Measurement of cholecystokinin in plasma with reference to nutrition related obesity studies. Nutrition Research. 2020 Apr 1;76: 1-8. https://doi.org/10.1016/j.nutres.2020.01.003.
4. Woodward OR, Gribble FM, Reimann F, Lewis JE. Gut peptide regulation of food intake–evidence for the modulation of hedonic feeding. The Journal of physiology. 2022 Mar;600(5):1053-78. https://doi.org/10.1113/JP2805815.
5. Aukan MI, Coutinho S, Pedersen SA, Simpson MR, Martins C. Differences in gastrointestinal hormones and appetite ratings between individuals with and without obesity—A systematic review and meta‐analysis. Obesity Reviews. 2023 Feb;24(2):13531. https://doi.org/10.1111/obr.13531.
6. Mastnak L, Herman R, Ferjan S, Janež A, Jensterle M. Prolactin in polycystic ovary syndrome: metabolic effects and therapeutic prospects. Life. 2023 Oct 26;13(11):2124. https://doi.org/10.3390/life13112124.
7. Yang H, Lin J, Li H, Liu Z, Chen X, Chen Q. Prolactin is associated with insulin resistance and beta-cell dysfunction in infertile women with polycystic ovary syndrome. Frontiers in Endocrinology. 2021 Feb 25;12: 571229. https://doi.org/10.3389/fendo.2021.571229.
8. Mekki S, Mohammed NS. The Impact of COVID-19 Infection on Gonadal Hormonal Functions in Iraqi Women. Journal of the Faculty of Medicine Baghdad. 2023;65(4). https://doi.org/10.32007/jfacmedbagdad.1988.
9. Ibrahim SK, Alsaffar SF. Assessment of Monocyte Chemoattractant Protein-1 and Fertility Hormones in Iraqi Women with Polycystic Ovarian Syndrome. IHJPAS. 2024;37(1):86-93. https://doi.org/10.30526/37.1.3307.
10. Misra, A., & Dhurandhar, N. V. Current formula for calculating body mass index is applicable to Asian populations. Nutrition & diabetes. (2019);9(1), 3. https://doi.org/10.1038/s41387-018-0070-9.
11. Fadhil NM. Evaluation of serum Podocalyxin in Iraqi women with polycystic ovary syndrome. J Fac Med Baghdad. 2022;64(4):276-9. https://doi.org/10.32007/jfacmedbagdad.6441983.
12. Hsu MI. Changes in the PCOS phenotype with age. Steroids. 2013 Aug 1;78(8):761-6. https://doi.org/10.1016/j.steroids.2013.04.005.
13. Mohapatra I, Samantaray SR. BMI and Polycystic Ovary Syndrome: Demographic Trends in Weight and Health. Cureus. 2024 Mar;16(3). https://doi.org/10.7759/cureus.55439.
14. Geary N, Asarian L, Graf G, Gobbi S, Tobler PN, Rehfeld JF, Leeners B. Increased Meal Size but Reduced Meal-Stimulated Plasma Cholecystokinin Concentrations in Women with Obesity. Endocrinology. 2023 Jan 1;164(1): BQAC192. https://doi.org/10.1210/endocr/bqac192.
15. Steinert RE, Feinle-Bisset C, Asarian L, Horowitz M, Beglinger C, Geary N. Ghrelin, CCK, GLP-1, and PYY (3–36): secretory controls and physiological roles in eating and glycemia in health, obesity, and after RYGB. Physiological reviews. 2017 Jan;97(1):411-63. https://doi.org/10.1152/physrev.00031.2014.
16. Emanuel RH, Roberts J, Docherty PD, Lunt H, Campbell RE, Möller K. A review of the hormones involved in the endocrine dysfunctions of polycystic ovary syndrome and their interactions. Frontiers in Endocrinology. 2022 Nov 15;13: 1017468. https://doi.org/10.3389/fendo.2022.1017468.
17. Cooper JA. Factors affecting circulating levels of peptide YY in humans: a comprehensive review. Nutrition research reviews. 2014 Jun;27(1):186-97. https://doi.org/10.1017/S0954422414000109.
18. Imamura M. Effects of surgical manipulation of the intestine on peptide YY and its physiology. Peptides. 2002 Feb 1;23(2):403-7. https://doi.org/10.1016/S0196-9781(01)00618-0.
19. Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA, Cone RD. Gut hormone PYY3-36 physiologically inhibits food intake. Nature. 2002 Aug 8;418(6898):650-4. https://doi.org/10.1038/nature00887.
20. Rasheed MK, Al-Naddawi AM. Association of Neuregulin-4 levels and body mass index with hyperandrogenism in Polycystic Ovary Syndrome patients. Journal of the Faculty of Medicine Baghdad. 2023;65(4). https://doi.org/10.32007/jfacmedbagdad.2140.
21. Paswan SK, Kumar R, Singh BK, Kumar D, Kumari S. To Study the Association Between Endocrinological and Metabolic Disorder in Case Both Obese and Non-Obese Polycystic Ovarian Syndrome. Int J Acad Med Pharm. 2023;5(5):512-6. https://doi.org/10.47009/jamp.2023.5.5.100.
22. Barber TM, Franks S. Obesity and polycystic ovary syndrome. Clinical endocrinology. 2021 Oct;95(4):531-41. https://doi.org/10.1111/cen.14421
23. Ali SI, Khaleel FM, Almukram AM. Association of ACE2, Insulin Resistance, and Other Parameters in Obese Polycystic Ovary Syndrome Patients Infected with COVID-19. Ibn AL-Haitham Journal For Pure and Applied Sciences. 2024 Jul 20;37(3):287-95. https://doi.org/10.32007/jfacmedbagdad.6421926.
24. Szlapinski, S. K., & Hill, D. J. Metabolic adaptations to pregnancy in healthy and gestational diabetic pregnancies: the pancreas-placenta axis. Current vascular pharmacology. 2021 19(2), 141-153. https://doi.org/10.2174/1570161118666200320111209
25. BA A, S. K., & P, S. M. (). General Endocrinology and Hormones of Hypothalamus and Pituitary. In Textbook of Veterinary Physiology. Singapore: Springer Nature Singapore. 2023 (pp. 369-390).https://doi.org/10.1007/978-981-19-9410-4_15.
26. Ascar IF, Hameed AS. Serum prolactin, Preptin, CCL 18 and genetic polymorphisms in Iraqi women with polycystic ovary syndrome. Baghdad Science Journal. 2021 Dec 20;18(4 (Suppl.)):1552-. https://dx.doi.org/10.21123/bsj.2021.18.4(Suppl.).1552.
27. Tomatis V, Battipaglia C, Genazzani AD. Thyroid, Adrenal, PRL Impairments and Ovarian Function. Endocrines. 2021 Jul 27;2(3):212-25. https://doi.org/10.3390/endocrines2030021
28. Yang H, Di J, Pan J, Yu R, Teng Y, Cai Z, Deng X. The association between prolactin and metabolic parameters in PCOS women: a retrospective analysis. Front. Endocrinol. 2020 May 12; 11:263. https://doi.org/10.3389/fendo.2020.00263.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Mariam A. Malik, Sura F. Alsaffar

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


