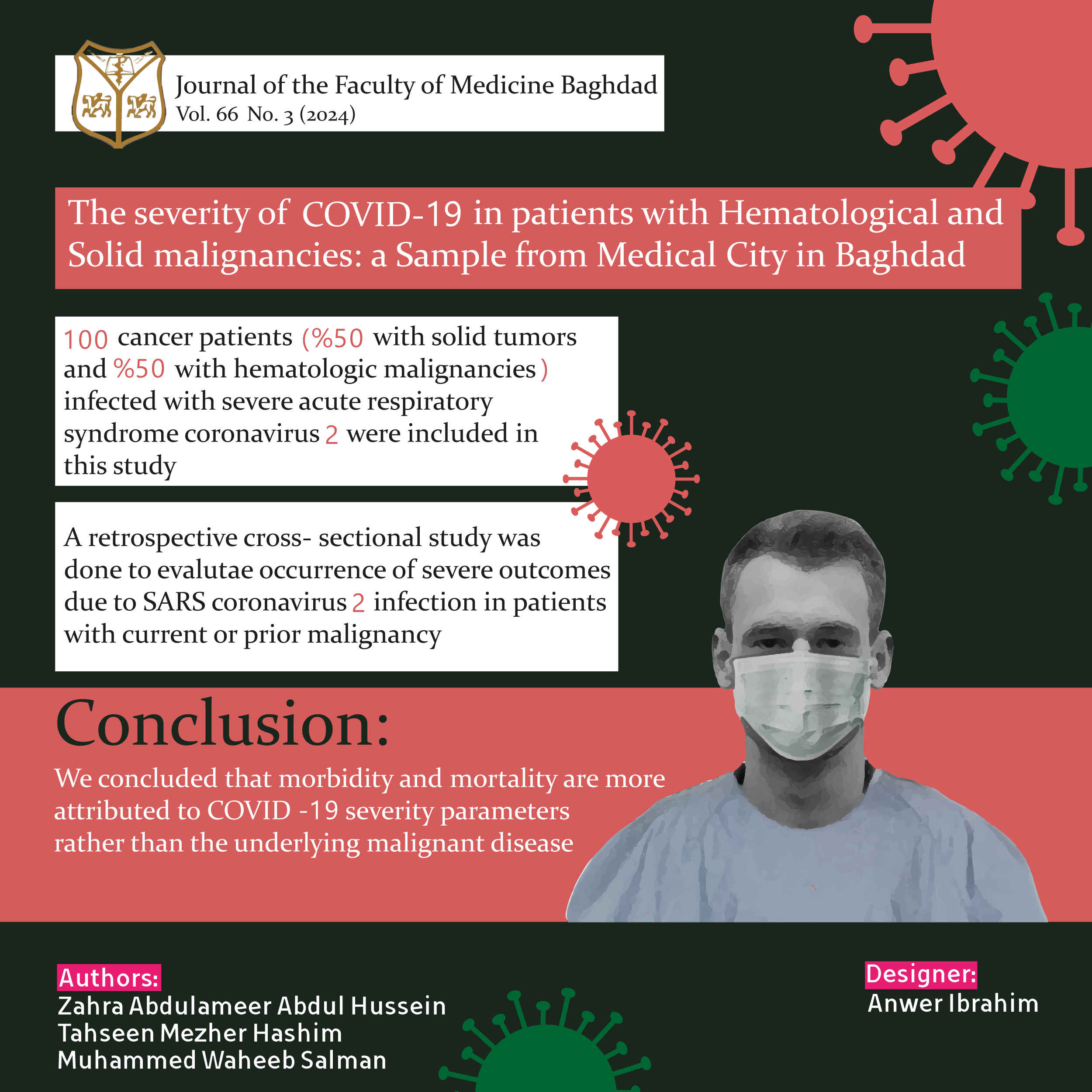
The Severity of COVID-19 in Patients with Hematological and Solid Malignancies: a Sample from Medical City in Baghdad.
DOI:
https://doi.org/10.32007/jfacmedbagdad.6612086الكلمات المفتاحية:
COVID-19;، Heamopiotic cancer; ، Iraqi malignant disease patients; ، Medical city complex; ، Sold cancerالملخص
تاثير جائحة كوفيد 19 على عينة من المرضى المصابين بالسرطان في العراق
الخلاصة:
خلفية الدراسة:
مرض فيروس كورونا 2019 (COVID-19) هو مرض فيروسي يسببه فيروس كورونا 2 (SARS-CoV-2) الجديد والمتلازمة التنفسية الحادة الوخيمة ويؤثر على الجهاز التنفسي للأفراد المصابين. ينتشر COVID-19 بين البشر من خلال الرذاذ التنفسي الذي ينتج عندما يسعل أو يعطس الشخص المصاب.
يتعرض الأفراد من جميع الأعمار لخطر الإصابة ، ولكن في معظم الحالات ترتبط شدة المرض بالعمر والأمراض الموجودة مسبقًا التي تهدد المناعة ، مثل السرطان.
الهدف من البحث:
في هذه الدراسة ، نقوم بتقييم معايير شدة عدوى COVID-19 لدى مرضى السرطان.
الطرق والمواد:
دراسة مقطعية بأثر رجعي تم جمعها خلال الفترة من كانون الثاني (يناير) إلى كانون الأول (ديسمبر) 2021 على 100 مريض مصاب بالسرطان (50٪ يعانون من أورام صلبة و 50٪ أورام دم خبيثة) من مراكز متعددة بما في ذلك مستشفى الأورام التعليمي ومركز بغداد لأمراض الدم ومستشفى دار التمريض الخاص في مجمع المدينة الطب.
النتائج:
كان هناك ارتباط ذي دلالة إحصائية بين شدة COVID-19 في مرضى السرطان ودرجة حالة أداء ECOG ≥1 (10٪ ، P = 0.009) ، ومدة الورم الخبيث ≥3 سنوات (30٪ ، P = 0.017) ، وحالة السرطان في وقت SARS-CoV-2 حيث وجد ان مرضى السرطان في حالة تعافي أثناء الإصابة بالفيروس التاجي أصيبوا بحالات أكثر خطورة (80 ٪ ، P = 0.001).
الاستنتاج:
تم استنتاج أن المراضة والوفيات تعزى بشكل أكبر إلى شدة معايير COVID-19 بدلاً من المرض الخبيث الأساسي.
الملخص الصوري
التنزيلات
المراجع
Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450-2. https://doi.org/10.1038/s41591-020-0820-9.
Li F. Structure, Function, and Evolution of Coronavirus Spike Proteins. Annu Rev Virol. 2016;3:237-61. https://doi.org/10.1146/annurev-virology-110615-042301.
Taylor D, Lindsay AC, Halcox JP. c or r e sp ondence Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. Nejm. 2020;0-2..
Yang Y, Yang M, Shen C, Wang F, Yuan J, Li J, et al. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. Innov. 2020;
https://doi.org/10.1101/2020.02.11.20021493.
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-NCoV). Radiology. 2020; 295(1):202-7. https://doi.org/10.1148/radiol.2020200230.
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020; 296(2):E32-40.
https://doi.org/10.1148/radiol.2020200642.
Mezalek ZT, Khibri H, Ammouri W, Bouaouad M, Haidour S, Harmouche H, et al. COVID-19 Associated Coagulopathy and Thrombotic Complications. Clin Appl Thromb. 2020; 26. https://doi.org/10.1177/1076029620948137.
Mucha SR, Dugar S, McCrae K, Joseph D, Bartholomew J, Sacha GL, et al. Update to coagulopathy in COVID-19: Manifestations and management. Cleve Clin J Med. 2020;1-10. https://doi.org/10.3949/ccjm.87a.ccc024-up.
Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020; 31: 894-901. https://doi.org/10.1016/j.annonc.2020.03.296.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21:335-7. https://doi.org/10.1016/S1470-2045(20)30096-6.
Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K, et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020; 21:904-13. https://doi.org/10.1016/S1470-2045(20)30467-8.
Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10:783-91.
https://doi.org/10.1158/2159-8290.CD-20-0422.
Garassino MC, Whisenant JG, Huang L-C, Trama A, Torri V, Agustoni F, et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol. 2020; 21:914-22. https://doi.org/10.1016/S1470-2045(20)30314-4.
Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020; 20:425-34.
https://doi.org/10.1016/S1473-3099(20)30086-4.
Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020; 382:1708-20. https://doi.org/10.1056/NEJMoa2002032.
Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020; 71: 769-77.https://doi.org/10.1093/cid/ciaa272.
Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID-19) infected patients. Br J Haematol. 2020;189: 428-37. https://doi.org/10.1111/bjh.16659.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506 https://doi.org/10.1016/S0140-6736(20)30183-5.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395:507-13.
https://doi.org/10.1016/S0140-6736(20)30211-7.
Hanna TP, Evans GA, Booth CM. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268-70. https://doi.org/10.1038/s41571-020-0362-6.
Muhammed Waheeb, Hassan M Abbas, et al. The first 40-days experience and clinical outcomes in the management of coronavirus covid-19 crisis. Single center preliminary study. J Fac Med Baghdad. 2020; 61:4-6. https://iqjmc.uobaghdad.edu.iq/index.php/19JFacMedBaghdad36/article/view/1739
Dockter AG, Angelos GC. Molecular-based alternatives for colorectal cancer screening during the COVID-19 pandemic. Surg Technol Int. 2020; 36:143-7. PMID: 32347964
Mohammed Waheeb Al‐Obaidy, Adnan Mohammed Al Jubouri, et al. Assessment of COVID-19 Treatment containing both Hydroxychloroquine and Azithromycin: A natural clinical trial. International Journal of Clinical Practice.2020; e13856. doi: https://doi.org/10.1111/ijcp.13856
Zacharia BE, Eichberg DG, Ivan ME, Hanft S, Boockvar JA, Isildak H, et al. Letter: surgical management of brain tumor patients in the COVID-19 era. Neurosurgery. 2020; 87:E197-200. https://doi.org/10.1093/neuros/nyaa162
Okwan-Duodu D, Pollack BP, Lawson D, Khan MK. Role of radiation therapy as immune activator in the era of modern immunotherapy for metastatic malignant melanoma. Am J Clin Oncol. 2015;38:119-25
https://doi.org/10.1097/COC.0b013e3182940dc3.
Macarulla T, Pazo-Cid R, Guillén-Ponce C, et al. Phase I/II trial to evaluate the efficacy and safety of nanoparticle albumin-bound paclitaxel in combination with gemcitabine in patients with pancreatic cancer and an ECOG performance status of 2. J Clin Oncol 2019; 37: 230-38. https://doi.org/10.1200/JCO.18.00089
J. Tian, X. Yuan, J. Xiao, Q. Zhong, C. Yang, B. Liu, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study Lancet Oncol, 21 (2020), pp. 893-903. https://doi.org/10.1016/S1470-2045(20)30309-0
Lee LYW, Cazier JB, Starkey T, Turnbull CD. UK Coronavirus Cancer Monitoring Project Team, Rachel Kerr, Gary Middleton COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020; 395:1919-1926.
https://doi.org/10.1016/S0140-6736(20)31173-9.
Liu C, Wang K, Li L, Lv Q, Liu Y, Hu T, Trent JC, Sun B, Hu Q. Severity of COVID-19 in cancer patients versus patients without cancer: a propensity score matching analysis. Journal of Cancer. 2021; 12(12):3558.https://doi.org/10.7150/jca.54205.
Zhang, H.; Han, H.; He, T.; Labbe, K.E.; Hernandez, A.V.; Chen, H.; Velcheti, V.; Stebbing, J.; Wong, K.K. Clinical Characteristics and Outcomes of COVID-19-Infected Cancer Patients: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2021, 113, 371-380. https://doi.org/10.1093/jnci/djaa168.
Lee LY, Cazier JB, Starkey T, Briggs SE, Arnold R, Bisht V, Booth S, Campton NA, Cheng VW, Collins G, Curley HM. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. The Lancet Oncology. 2020 Oct 1;21(10):1309-16.
https://doi.org/110.1016/S1470-045(20)30442-3
Crolley VE, Hanna D, Joharatnam-Hogan N, Chopra N, Bamac E, Desai M, Lam YC, Dipro S, Kanani R, Benson J, Wilson W. COVID-19 in cancer patients on systemic anti-cancer therapies: outcomes from the CAPITOL (COVID-19 Cancer PatIenT Outcomes in North London) cohort study. Therapeutic advances in medical oncology. 2020 Oct; 12: https://doi.org/10.1177/1758835920971147
Vikas Mehta,,Sanjay Goal, Rafi .K ,et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system Cancer Discov, 10 (7) (2020), pp. 935-941.
Liu C, Wang K, Li L, Lv Q, Liu Y, Hu T, Trent JC, Sun B, Hu Q. Severity of COVID-19 in cancer patients versus patients without cancer: a propensity score matching analysis. Journal of Cancer. 2021; 12(12):3558.https://doi.org/10.7150/jca.54205.
Vikas Mehta,,Sanjay Goal, Rafi .K ,et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system Cancer Discov, 10 (7) (2020), pp. 935-941. DOI: https://doi.org/110.1158/2159-8290.CD-20-0516
Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, Chackathayil J, Cheng VW, Curley HM, Fittall MW, Freeman-Mills L. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. The Lancet. 2020 Jun 20; 395(10241):1919-26.https://doi.org/10.1016/S0140-6736(20)31173-9.
Mohammed Waheeb AL-Obaidy, Adnan Mohammed Al Jubouri,et al. Presenting the characteristics, smoking versus diabetes, and outcome among patients hospitalized with COVID-19, Journal of Medical Virology.2020; https://onlinelibrary.wiley.com/doi/abs/10.1002/jmv.26487.
Antrim L, Capone S, Dong S, Chung D, Lin S, Wald-Dickler N, In GK. Impact of COVID-19 infection among cancer patients treated at the Los Angeles County Medical Center. Cancer Treatment and Research Communications. 2021 Jan 1; 26: 100273 https://doi.org/10.1016/j.ctarc.2020.100273.
Lima, A.; Sousa, H.; Nobre, A.; Faria, A.L.; Machado, M. The Impact of COVID-19 Pandemic in Portuguese Cancer Patients: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 8552. https://doi.org/10.3390/ijerph18168552.
Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med 2020; 382: 1653-59.
التنزيلات
الملفات الإضافية
منشور
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Muhammed Waheeb Salman AL-Obaidy, Mudher Al-Khairalla,Zahra Abdulameer Abdul Hussein,Tahseen M. Hashim.

هذا العمل مرخص بموجب Creative Commons Attribution 4.0 International License.

















 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


