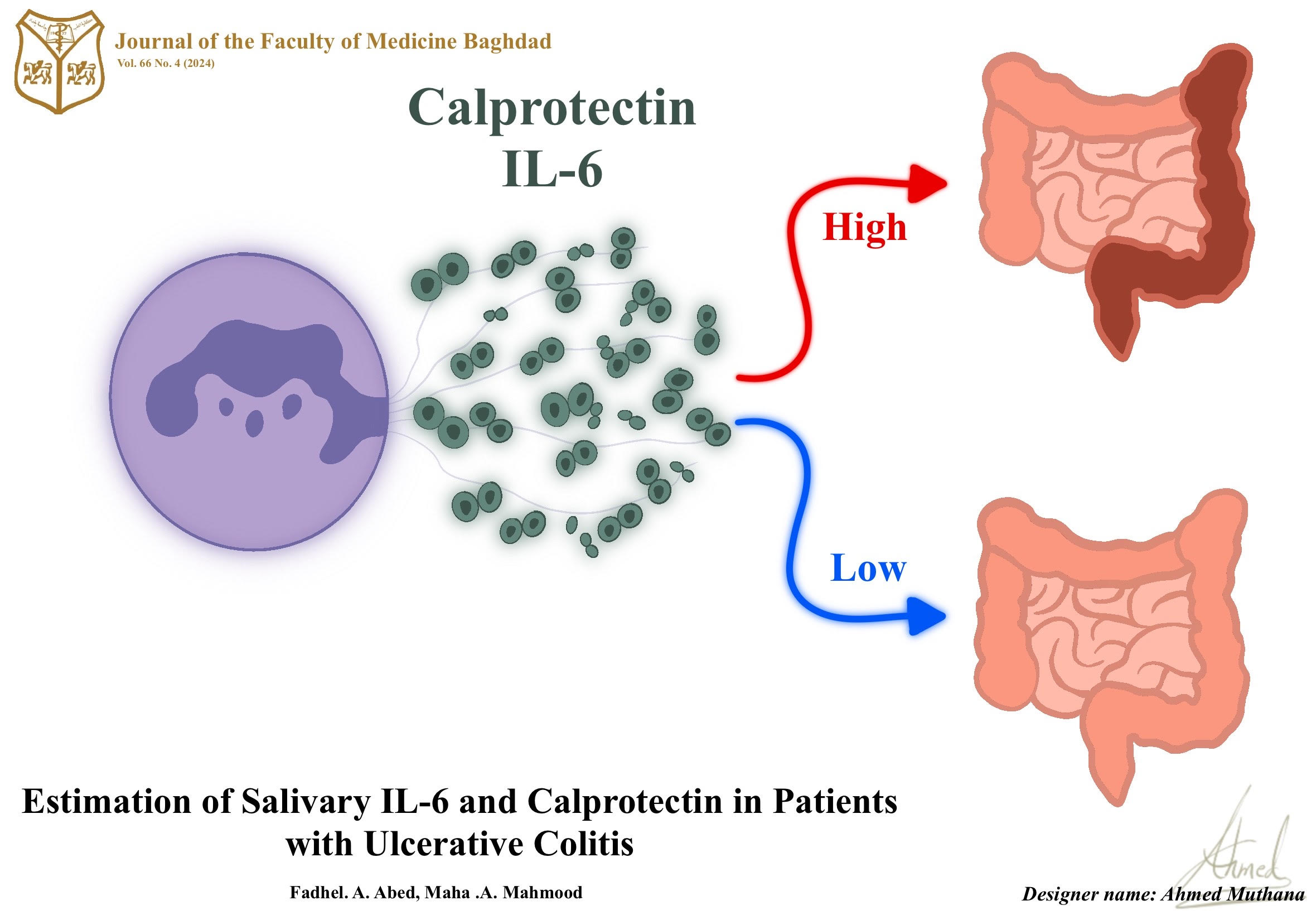
Estimation of salivary IL-6 and calprotectin in patients with ulcerative colitis
DOI:
https://doi.org/10.32007/jfacmedbagdad.6612031الكلمات المفتاحية:
Salivary IL-6, calprotectin, ulcerative colitisالملخص
Inflammatory bowel disease (IBD) is chronic inflammation of the gastrointestinal tract (GIT) it includes two-condition Crohn’s disease (CD) and ulcerative colitis (UC) the prolonged inflammation may cause invasion of the multiple layers of the intestinal walls result in GIT damage. The current study was carried out in Baghdad teaching hospital and gastroenterology hospital from November 2021 to May 2022. In order to show if the diagnostic marker of IBD which are IL6& calprotectin are rises in saliva as in sera and if there are significant differences in the levels of those markers between UC patients and healthy control subjects.
The subjects included twenty five patients suffering from ulcerative colitis and twenty five healthy individuals representing the control group. All of them having ages ranged between 20-55 years.
The recent study was measured the levels of Interleukin-6 (IL-6) and calprotectin in saliva of UC patients using ELISA method.
The present results showed a significant increase in the levels of both (IL-6) and calprotectin in UC patients when compared with that of control group (P=<0.05).Moreover, this study was found a significant positive correlation between IL-6 levels and age in all study groups (UC and control) (P <0.05) and between IL-6 and calprotectin in UC patients(p<0.05).
التنزيلات
المراجع
1. Abdul-Hussein SS, et al. Roles of IL-17A and IL-23 in the Pathogenesis of Ulcerative Colitis and Crohn’s Disease. Iraqi Journal of Science. 2021; 2526-2535. https://doi.org/10.24996/ijs.2021.62.8.5.
2. Frøslie KF, et al. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007; 133(2): 412-422. https://doi.org/10.1053/j.gastro.2007.05.05.
3. Manna MJ, Abu-Raghif A, Al-Saree OJAH. The value of doxycycline in acetic acid induce ulcerative colitis in rats. IJPSR. 2018; 9(8): 3567-3572. http://dx.doi.org/10.13040/IJPSR.0975-8232.9(8).3567-72.
4. Abdal-Zahra N, et al. The significance of miR-196a2 C< T single nucleotide polymorphism and serum levels of interleukin-1β (IL-1β) and interleukin-6 (IL-6) in colorectal cancer. JPharmSciRes. 2019; 11(4): 1652-165. https://doi.org/10.1016/j.mgene.2017.02.004.
5. Al-Hassan AA. Possible association of HLA class I and II molecules with Ulcerative colitis in Iraqi patients. Iraqi Journal of Medical Sciences. 2008; 6 (1).https://www.iasj.net/iasj/download/4cde74b676b80148
6. Daham KJ, Hamel KI, Khorsheed SA. Management of ulcerative colitis in a sample of Iraqi patients. International Journal of Surgery. 2019; 3(3):344-348. https://doi.org/10.33545/surgery.2019.v3.i3f.192.
7. Surcel M, et al. Inflammatory cytokine pattern is sex-dependent in mouse cutaneous melanoma experimental model. Journal of Immunology Research. 2017; 2017. https://doi.org/10.1155/2017/9212134.
8. Gabay C. Interleukin-6 and chronic inflammation. Arthritis research & therapy. 2006; 8(2): 1-6. https://doi.org/10.1186/ar1917
9. Juda TM, Beder S, Zaidan KI. Salivary Interleukine 6 and its role on developing periodentitis. Irq. Nat. J. Chem. 2016;16(1):22-31. https://injchemistry.uobabylon.edu.iq/index.php/chem/article/view/703/648
10. Larsen TB, et al. Platelets and anticoagulant capacity in patients with inflammatory bowel disease. Pathophysiology of Haemostasis and Thrombosis. 2002; 32(2): 92-96. https://doi.org/10.1159/000065082.
11. Al-Tameemi S, et al. Calprotectin may be positively associated with the severity of acne vulgaris. BJBiochemistry and Applied Biological Sciences. 2022; 3(02): 145-155. https://doi.org/10.47419/bjbabs.v3i02.124.
12. Wei L, Liu M, Xiong H. Role of calprotectin as a biomarker in periodontal disease. Mediators of Inflammation. 2019; 2019. https://doi.org/10.1155/2019/3515026.
13. Ostrowska L, et al. Which salivary components can differentiate metabolic obesity?. PLoS One. 2020; 15 (6): e0235358. https://doi.org/10.1371/journal.pone.0235358.
14. Gilat D. The best bound in the inequality of Hardy and Littlewood and its martingale counterpart. Proceedings of the American Mathematical Society. 1986; 97(3): 429-436. https://doi.org/10.1090/S0002-9939-1986-0840624-3
15. Hassan JT, Delmany AS. Epidemiological and clinical characteristics of patients with inflammatory bowel disease in Erbil City. Medical Journal of Babylon. 2018 Oct 1;15(4):281-5. https://doi.org/10.4103/MJBL.MJBL_65_18
16. Hammasur GA, Mohammed FO, Ahmad AJ. Assessment of rock slope stability along Sulaimaniyah-Qaradagh main road, near Dararash Village, Sulaimaniyah, NE-Iraq. Iraqi Journal of Science. 2020; 3266-3286. https://doi.org/10.24996/ijs.2020.61.12.15.
17. Hirano T. Interleukin 6 and its receptor: ten years later. International Reviews of Immunology. 1998; 16(3-4): 249-284. https://doi.org/10.3109/08830189809042997.
18. Atreya R, et al. Blockade of interleukin 6 trans signaling suppresses T-cell resistance against apoptosis in chronic intestinal inflammation: evidence in Crohn disease and experimental colitis in vivo. Nature Medicine. 2000; 6(5): 583-588. https://doi.org/10.1038/75068.
19. Baumann H, Gauldie J. The acute phase response. Immunology Today. 1994; 15(2): 74-80. https://doi.org/10.1016/0167-5699(94)90137-6.
20. Mazlam MZ, Hodgson HJ. Interrelations between interleukin-6, interleukin-1 beta, plasma C-reactive protein values, and in vitro C-reactive protein generation in patients with inflammatory bowel disease. Gut. 1994; 35(1): 77-83. https://doi.org/10.1136/gut.35.1.77.
21. Nielsen AA, et al. Saliva interleukin-6 in patients with inflammatory bowel disease. Scandinavian Journal of Gastroenterology. 2005; 40(12): 1444-1448. https://doi.org/10.1080/00365520510023774.
22. Al-Mudhaffer MH, Abdul-Ghafoor SH. Salivary assessment of interleukin-6, C-reactive protein, and albumin in ulcerative colitis patients in relation to oral findings. Journal of Baghdad College of Dentistry. 2013; 325(2204): 1-5. https://doi.org/10.12816/0014972.
23. Majster M, Almer S, Boström EA. Salivary calprotectin is elevated in patients with active inflammatory bowel disease. Archives of Oral Biology. 2019; 107: 104528. https://doi.org/10.1016/j.archoralbio.2019.104528.
24. Bjerke K, et al. Distribution of macrophages and granulocytes expressing L1 protein (Calprotectin) in human Peyer's patches compared with normal ileal lamina propria and mesenteric lymph nodes. Gut. 1993; 34(10): 1357-1363. https://doi.org/10.1136/gut.34.10.1357.
25. Fagerberg UL, et al. Fecal Calprotectin levels in healthy children studied with an improved assay. Journal of Pediatric Gastroenterology and Nutrition. 2003; 37(4): 468-472. https://doi.org/10.1097/00005176-200310000-00013.
26. Burak S, Margat J. Water management in the Mediterranean region: concepts and policies. Water Resources Management. 2016; 30(15): 5779-5797. https://doi.org/10.1007/s11269-016-1389-4.
27. Zhou HJ, et al. Validation of the functional assessment of cancer therapy-gastric module for the Chinese population. Health and Quality of Life Outcomes. 2012; 10(1): 1-8. https://doi.org/10.1186/1477-7525-10-145.
28. Shah SC, Khalili H, Gower-Rousseau C, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from western countries. Gastroenterology. 2018; 155: 1079–1089. https://doi.org/10.1053/j.gastro.2018.09.014.
29. Shah SC, Khalili H, Chen CY, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from the Asia-Pacific region. Aliment Pharmacol Ther. 2019; 49: 904–911. https://doi.org/10.1111/apt.15178.
30. Nijakowski K, Surdacka A. Salivary Biomarkers for Diagnosis of Inflammatory Bowel Diseases: A Systematic Review. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21207477.
31. Nijakowski K, Surdacka A. Salivary Biomarkers for Diagnosis of Inflammatory Bowel Diseases: A Systematic Review. Int J Mol Sci. 2020; 21:7477. https://doi.org/10.3390/ijms21207477.
32. Szczeklik K, Owczarek D, Pytko-Polónczyk J, Kęsek B, Mach TH. Proinflammatory Cytokines in the Saliva of Patients with Active and Non-Active Crohn’s Disease. Pol Arch Med Wewn. 2012; 122:200-208. https://doi.org/10.20452/pamw.1256.
33. Dobre M, et al. Differential Intestinal Mucosa Transcriptomic Biomarkers for Crohn’s Disease and Ulcerative Colitis. Journal of Immunology Research. 2018. https://doi.org/10.1155/2018/9208274.
التنزيلات
الملفات الإضافية
منشور
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2024 Fadhel Abdullah, Maha

هذا العمل مرخص بموجب Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


