The Role of Omentin-1 and Fibroblast Growth Factor-23 in Iraqi Patients with Prostate Cancer during Chemotherapy
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632256Keywords:
Prostate cancer, Chemotherapy, Omentin-1, FGF-23, IrisinAbstract
Background: Omentin-1 is mainly expressed in stromal vascular cells of adipose tissue and can also be expressed in airway goblet cells, mesothelial cells, and vascular cells. Fibroblast growth factor 23 (FGF-23), generated by bone cells, regulates phosphate and vitamin D metabolism by regulating phosphate reabsorption in the kidneys and inhibiting vitamin D activation. Vitamin D is a fat-soluble vitamin that regulates calcium absorption, bone health, and immunological function. Prostate cancer is a significant health concern for men worldwide. Several studies demonstrated a link between these variables and cancer as they exert important anti-inflammatory, antioxidative, and anti-cancer functions.
Objectives: To assess the impact of Omentin and FGF-23 biochemical functions, as well as the anti-cancer properties of vitamin D.
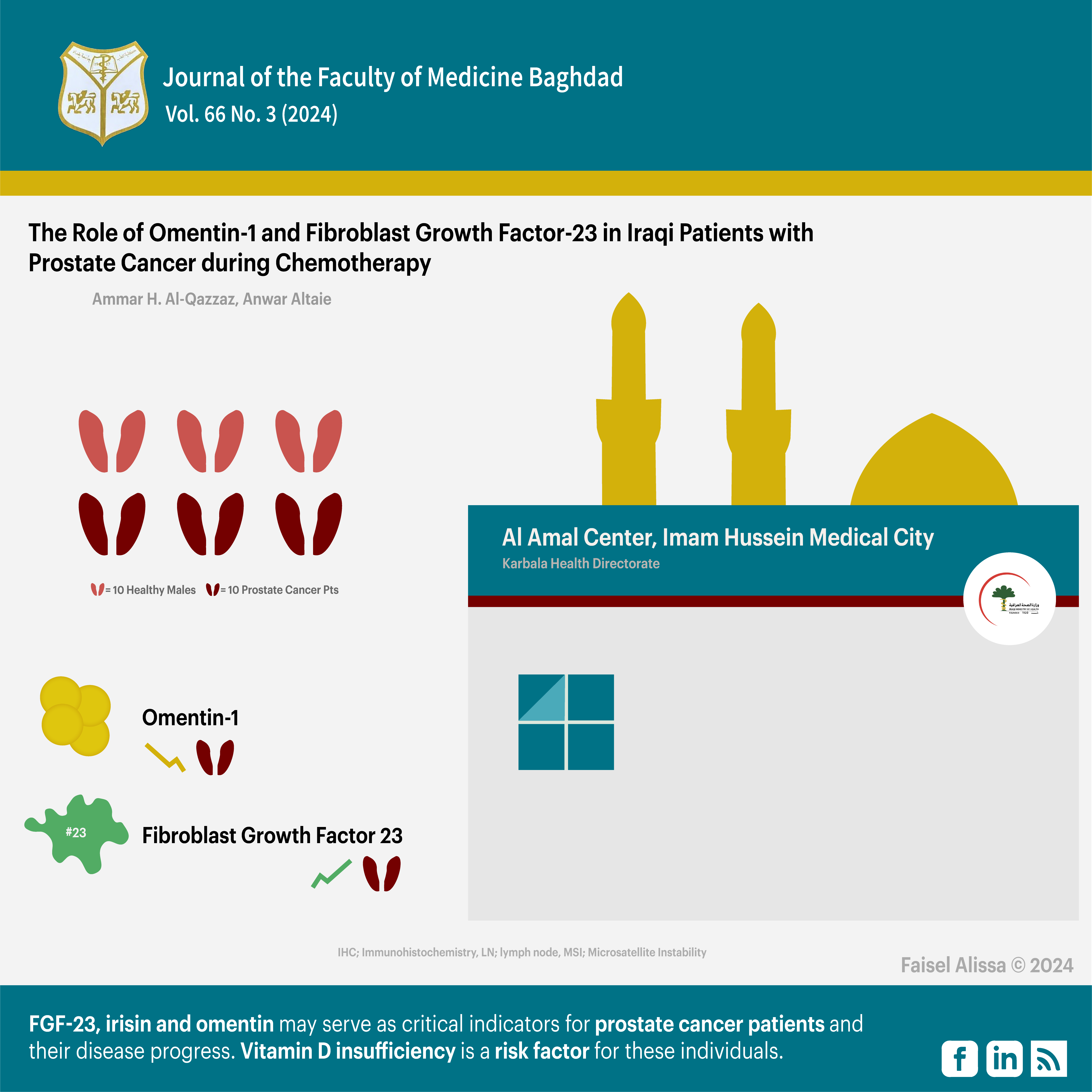
Subjects and methods: This is a case-control study on serum samples collected from Iraqi prostate cancer patients after receiving chemotherapy at Al Amal Center in Imam Hussein Medical City in Karbala between November 2022 to May 2023. The serum samples were collected from two groups: control group consisted of 30 healthy males. Patient group consisted of 30 prostate cancer patients after receiving chemotherapy, both groups aged 45 – 80 years. The two groups were matched for body mass index. ELISA technology was used to estimate serum levels of the aforementioned biochemical parameters with vitamin D.
Results: patient group had a significantly higher FGF-23 level than control group (309.5±41.65) versus (163.1±22.4) (p<0.001). On the other hand, Irisin, Omentin and Vitamin D mean serum concentrations were significantly lower in-patient group (15.2±4.24), (13.8±4.28) and (4.4±0.69) (p<0.001), respectively, compared to control group (60.8±3.5), (38.8±6.59), and (18.9±2.36), respectively. (ROC) curve analysis identified the best AUC values of FGF-23, Omentin, and Vitamin D (0.995, 0.959, 0.937), respectively, which suggests a high level of accuracy.
Conclusions: These parameters may serve as critical indicators for prostate cancer patients and their disease progress. Vitamin D insufficiency is a risk factor for these individuals.
Received: Dec, 2023
Revised: March 2024
Accepted: May 2024
Downloads
References
Varaprasad GL, Gupta VK, Prasad K, Kim E, Tej MB, Mohanty P, et al. Recent advances and future perspectives in the therapeutics of prostate cancer. Experimental Hematology & Oncology. 2023 Sep 22;12(1):80. https://doi.org/10.1186/s40164-023-00444-9
Razaghi A, Heimann K, Schaeffer PM, Gibson SB. Negative regulators of cell death pathways in cancer: perspective on biomarkers and targeted therapies. Apoptosis. 2018;23(2):93-112. https://doi.org/10.1007/s10495-018-1440-4
Bleyer A, Spreafico F, Barr R. Prostate cancer in young men: An emerging young adult and older adolescent challenge. Cancer. 2020 Jan 1;126(1):46-57. https://doi.org/10.1002/cncr.32498
Badal S, Aiken W, Morrison B, Valentine H, Bryan S, Gachii A, et al. Disparities in prostate cancer incidence and mortality rates: Solvable or not?. The Prostate. 2020 Jan;80(1):3-16. https://doi.org/10.1002/pros.23923
James LJ, Wong G, Craig JC, Hanson CS, Ju A, Howard K, et al. Men’s perspectives of prostate cancer screening: A systematic review of qualitative studies. PloS one. 2017;12(11):e0188258. https://doi.org/10.1371/journal.pone
National Cancer Institute. SEER Cancer stat facts: prostate cancer.https://seer.cancer.gov/statfacts/html/prost.html
Ahmed HS, Salman ED. Role of Serum Omentin-1 and Bone Metabolism Markersin Osteoporosis among Postmenopausal Women. Annals of the Romanian Society for Cell Biology. 2021;25(6):8317-27. https://annalsofrscb.ro/index.php/journal/article/view/7025
Tao M, Yan W, Chen C, Tang M, Zhao X, Feng Q, et al. Omentin-1 ameliorates experimental inflammatory bowel disease via Nrf2 activation and redox regulation. Life Sciences. 2023;328:121847. https://doi.org/10.1016/j.lfs.2023.121847
Kadium TE, Alrubaie A, Ghanim Samjbsj. The Link between Serum Omentin Level and Insulin Resistance Biomarkers, Lipid Profile, and Atherogenic Indices in Iraqi Obese Patients. Baghdad Science Journal. 2023;20(1):0074-. https://dx.doi.org/10.21123/bsj.2022.6535
Ali IA, Ali SH. Impact of osteocalcin level on vascular calcification in type 2 diabetics in relation to fibroblast growth factor-23 (FGF-23). Iraqi Journal of Pharmaceutical Sciences. 2018:42-54. https://doi.org/10.31351/vol27iss2pp42-54
Thajeel TS, Rasheed MK, Sudany A, Hanon MJB. Evaluation of cystatin c and fibroblast growth factor 23 in type 2 diabetic patients and its association with early nephropathy. Biochemical & Cellular Archives. 2021;21(1). https://connectjournals.com/03896.2021.21.1429
Ameen ZA, Ali SH. Effects of Aldosterone, Osteoprotegerin and Fibroblast Growth Factor-23 and Some Biochemical Markers in Chronic Kidney Disease Patients (Stage II-IV) among Patients with or without Cardiovascular Events. Iraqi Journal of Pharmaceutical Sciences. 2018;27(2):150-8. https://doi.org/10.31351/vol27iss2pp150-158
Colangelo L, Sonato C, Cipriani C, Pepe J, Farinacci G, Palmisano B, et al. Occipital bone and tumor-induced osteomalacia: a rare tumor site for an uncommon paraneoplastic syndrome. Archives of Osteoporosis. 2023;18(1):94. https://doi.org/10.1007/s11657-023-01305-y
Al-Khaykanee AM, Abdel-Rahman AA, Essa A, Gadallah A-NA-A, Ali BH, Al-Aqar AA, et al. Genetic polymorphism of fibroblast growth factor receptor 2 and trinucleotide repeat-containing 9 influence the susceptibility to HCV-induced hepatocellular carcinoma. Clinics and Research in Hepatology and Gastroenterology 2021;45(6):101636. https://doi.org/10.1016/j.clinre.2021.101636
Alkhader RA, Ali KAW, Al-Kharasani AM. Irisin levels related to glycosylated hemoglobin in type 2 diabetic obese women. Iraqi Journal of Science. 2020:2150-5. https://doi.org/10.24996/ijs.2020.61.9.1
Sattar AA, Warka'a TJ. Evaluation of Adiponectin, Irisin, Vitamin D Levels and Their Relation in Iraqi Patients with Non alcoholic Fatty Liver Disease. Ibn AL-Haitham Journal For Pure and Applied Sciences. 2023;36(2):241-50. https://doi.org/10.30526/36.2.3043
Al-Aridhi DTN, Allehibi KIH, Al-Sharifi ZA, Al Quraishi MJM-LU. Serum Levels of Novel Biochemical Marker (Irisin) in Relation to the Duration of Type 2 Diabetes & in Cases of Type 2 diabetes with Coronary Artery Disease in Iraqi Patients Aged (40-60 year). Medico-Legal Update. 2020;20(1). https://doi.org/10.37506/v20%2Fi1%2F2020%2Fmlu%2F194390
Kuloğlu T, Artaş G, Yardim M, Aydin Y, Beyoğlu N, Özercan İ, et al. Immunostaining characteristics of irisin in benign and malignant renal cancers. Biotechnic & Histochemistry. 2019;94(6):435-41. https://doi.org/10.1080/10520295.2019.1586998
Cebulski K, Piotrowska A, Kmiecik A, Haczkiewicz-Leśniak K, Ciesielska U, Grzegrzółka J, et al. The Role of Irisin/FNDC5 Expression and Its Serum Level in Breast Cancer. International Journal of Molecular Sciences. 2023;24(10):8628. https://doi.org/10.3390/ijms24108628
Alshanqiti KH, Alomar SF, Alzoman N, Almomen AJC. Irisin induces apoptosis in metastatic prostate cancer cells and inhibits tumor growth in vivo. Cancers. 2023;15(15):4000. https://doi.org/10.3390/cancers15154000
Roni SM, Djajadikerta HG. Data analysis with SPSS for survey-based research: Springer; 2021. https://doi.org/10.1007/978-981-16-0193-4
Tekin S, Erden Y, Sandal S, Yilmaz BJ. Is irisin an anticarcinogenic peptide? Medicine Science. 2015;4(2):2172-80. https://dx.doi.org/10.5455/medscience.2014.03.8210
Aslan R, Alp HH, Eryılmaz R, Huyut Z, Sevim M, Araz Ş, et al. Can the irisin be a biomarker for prostate cancer? A case control study. 2020;21(2):505. https://doi.org/10.31557%2FAPJCP.2020.21.2.505
Huh JY, Panagiotou G, Mougios V, Brinkoetter M, Vamvini MT, Schneider BE, et al. FNDC5 and irisin in humans: I. Predictors of circulating concentrations in serum and plasma and II. mRNA expression and circulating concentrations in response to weight loss and exercise. Metabolism. 2012;61(12):1725-38. https://doi.org/10.1016/j.metabol.2012.09.002
Kashash SA, Hameed AS. Evaluating the Fibroblast Growth Factor-23 and Phosphate in Iraqi Patients with Acromegaly. Baghdad Science Journal. 2024;21(3). https://doi.org/10.21123/bsj.2023.8814
Nakatani S, Nakatani A, Mori K, Emoto M, Inaba M, Razzaque MS. Fibroblast growth factor 23 as regulator of vitamin D metabolism. Phosphate Metabolism: From Physiology to Toxicity: Springer; 2022; p. 47-54. https://doi.org/10.1007/978-3-030-91623-7_6
Mizuno Y, Ishida T, Kugimiya F, Takai S, Nakayama Y, Yonemitsu K, et al. Deterioration of Phosphate Homeostasis Is a Trigger for Cardiac Afterload―Clinical Importance of Fibroblast Growth Factor 23 for Accelerated Aging―. Circulation Reports. 2023;5(1):4-12. https://doi.org/10.1253/circrep.CR-22-0124
Teishima J, Hayashi T, Nagamatsu H, Shoji K, Shikuma H, Yamanaka R, et al. Fibroblast growth factor family in the progression of prostate cancer. Journal of Clinical Medicine. 2019;8(2):183. https://doi.org/10.3390/jcm8020183
Hussain A, Tripathi A, Pieczonka C, Cope D, McNatty A, Logothetis C, et al. Bone health effects of androgen-deprivation therapy and androgen receptor inhibitors in patients with nonmetastatic castration-resistant prostate cancer. Prostate cancer and prostatic diseases. 2021;24(2):290-300. https://doi.org/10.1038/s41391-020-00296-y
Sekhoacha M, Riet K, Motloung P, Gumenku L, Adegoke A, Mashele SJM. Prostate cancer review: Genetics, diagnosis, treatment options, and alternative approaches. Molecules. 2022;27(17):5730. https://doi.org/10.3390/molecules27175730
Borowski A, Sieminska L. Serum Omentin Levels in Patients with Prostate Cancer and Associations with Sex Steroids and Metabolic Syndrome. J Clin Med. 2020;9(4):1179. https://doi.org/10.3390%2Fjcm9041179
Reckell T, Nguyen K, Phan T, Crook S, Kostelich EJ, Kuang Y. Modeling the synergistic properties of drugs in hormonal treatment for prostate cancer. J Theor Biol. 2021;514:110570. https://doi.org/10.1016/j.jtbi.2020.110570
Ismail NH, Mussa A, Al-Khreisat MJ, Mohamed Yusoff S, Husin A, Johan MF, et al. The Global Prevalence of Vitamin D Deficiency and Insufficiency in Patients with Multiple Myeloma: A Systematic Review and Meta-Analysis. Nutrients. 2023;15(14):3227. https://doi.org/10.3390/nu15143227
Al-Mendalawi MD. Correlation of Vitamin D3 Levels with Disease Severity in Psoriasis Patients–A Case-Control Study. Indian Journal of Dermatology. 2023 May 1;68(3):356. https://doi.org/10.4103/ijd.ijd_211_23
Moslem MN, Altaie A. Correlation study of (IL-17, IL-17RA) and some biochemical parameters with patients of Iraq colorectal cancer after and before taking a dose of chemotherapy. AIP Conference Proceedings. 2020;2213(1). https://doi.org/10.1063/5.0000066
Rondanelli M, Moroni A, Zese M, Gasparri C, Riva A, Petrangolini G, et al. Vitamin D from UV-Irradiated Mushrooms as a Way for Vitamin D Supplementation: A Systematic Review on Classic and Nonclassic Effects in Human and Animal Models. Antioxidants. 2023;12(3):736. https://doi.org/10.3390/antiox12030736
Hussein TA, Shafeeq NK, Hussain NA. Comparison of 1, 25-Dihydroxyvitamin D3 and Glutathione Reductase Levels in Thyroid Gland Patients. Pakistan Journal of Medical and Health Sciences. 2021;15(1):224 - 9. https://pjmhsonline.com/2021/jan/224.pdf
Abass EJ. Vitamin D level and its relation with the newly diagnosed diabetic neuropathy in women with hypothyroidism. Archives of Razi Institute. 2022;77(3):1139. https://doi.org/10.22092%2FARI.2022.357389.2029
Carlberg C, Raczyk M, Zawrotna N. Vitamin D: A master example of nutrigenomics. Redox Biol. 2023;62:102695. https://doi.org/10.1016/j.redox.2023.102695
Seraphin G, Rieger S, Hewison M, Capobianco E, Lisse TS. The impact of vitamin D on cancer: A mini review. J Steroid Biochem Mol Biol. 2023;231:106308. https://doi.org/10.1016/j.jsbmb.2023.106308
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Ammar H. Al-qazzaz, Anwar F. Altaie

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


