Oral Findings and Salivary Alpha-Amylase in Major Depressive Disorder Patients
DOI:
https://doi.org/10.32007/jfacmedbagdad.6622188Keywords:
Altered taste, Burning Mouth syndrome, Major depressive disorder, Recurrent Oral ulcerations, Salivary Alpha-amylaseAbstract
Background: The increasing global prevalence of major depressive disorder (MDD) has become an important challenge, leading to a heightened demand for oral medicine in developed nations. This demand arises from the recognition of the association between psychiatric disorders and other conditions, including various orofacial pain disorders.
Objective: This study are to evaluate oral conditions such as recurrent aphthous ulcers, burning mouth syndrome, and altered taste and to assess salivary alpha-amylase in individuals diagnosed with major depressive disorder.
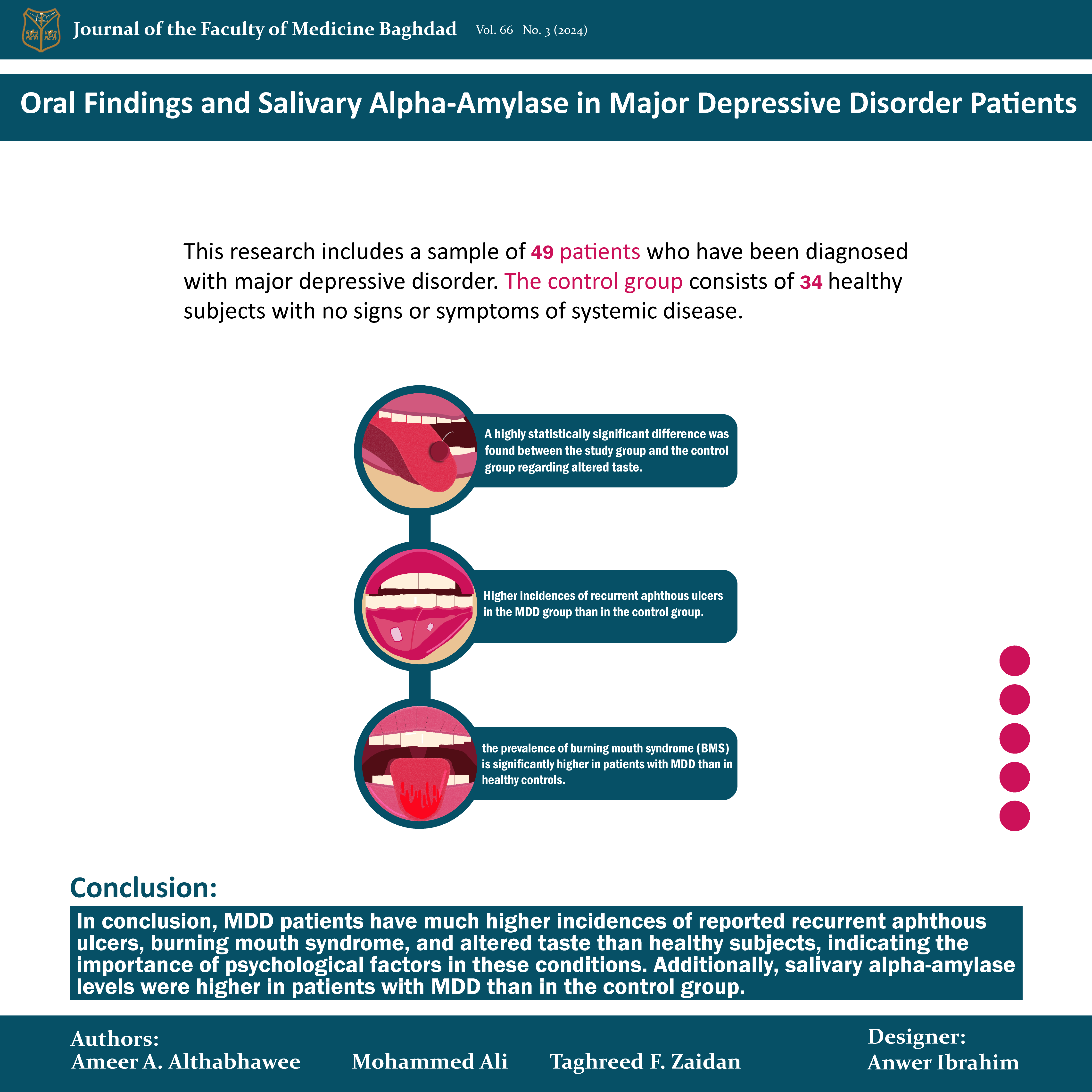
Methods: This research uses a cross-sectional study design that includes a sample of 49 patients who have been diagnosed with major depressive disorder and who have undergone treatment for at least two weeks. The control group consists of 34 healthy subjects with no signs or symptoms of systemic disease. The study group received the diagnosis in Najaf City according to the criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). With respect to recurrent aphthous ulcers, the results of this study show the percentage of patients with oral ulcers is significantly higher than in the control group.
Results: The results also show that the prevalence of burning mouth syndrome is significantly higher in patients with major depressive disorder than in healthy controls. A highly statistically significant difference was found between the study group and the control group regarding altered taste. There is also a significant difference in salivary alpha-amylase levels between the study and control groups (p = 0.009).
Conclusion: Major depressive disorder patients have much higher incidences of reported recurrent aphthous ulcers, burning mouth syndrome, and altered taste than healthy subjects, indicating the importance of psychological factors in these conditions. Additionally, salivary alpha-amylase levels were higher in patients with major depressive disorder than in the control group.
Received: July, 2023
Revised: Jan. 2024
Accepted: April 2024
Published: July. 2024
Downloads
References
Monroe Sm, Harkness Kl. Major Depression and Its Recurrences: Life Course Matters. Annu Rev Clin Psychol [Internet]. 2022;18(1):329–57. https://doi.org/10.1146/annurevclinpsy072220021440
Ibrahim AA, Ailami F, AlRudainy R, Khader Ys. Mental Disorders Among Elderly People in Baghdad, Iraq, 2017. INQUIRY. 2019;56:0046958019845960. https://doi.org/10.1177/0046958019845960
Saad A, Ogden R, Falaiyah, Ashraf M, Sayyid A, Abbas A. The passage of time in Iraq during the covid19 pandemic. PLOS ONE. 2022 14;17(4):e0266877-. https://doi.org/10.1371/journal.pone.0266877
Aljuboori SB, Sahar B, Azeez A, Mahmood, Fathel R, Talab H. Evaluate factors influencing depression in Baghdad: Using DeckDepression Inventory. Innovations in Pharmacy. 2019;10(3). https://doi.org/10.24926/iip.v10i3.2036
Kathem SH, Sarmed H, AlJumail A, NoorAldeen M, Najah N, Khalid A. Measuring depression and anxiety prevalence among Iraqi healthcare college students using hospital anxiety and depression scale. Pharmacy Practice (Granada). 2021;19(2). https://doi.org/10.18549/PharmPract.2021.2.2303
Jaber Za, Salman Rt, Abid Al Wahab Dy, Habib Ma, Hussein Ia. Assessment of the Depression Level among Medical Students at University of Baghdad, College of Medicine. kMJ. 2021 Dec 30;17(3):175–9. https://doi.org/10.47723/kcmj.v17i3.248
Shawi A, Hameed Ak, Shalal, Aatika I, Sara K, Majeed Ma, Humidy St. Internet Addiction and Its Relationship to Gender, Depression and Anxiety Among Medical Students in Anbar GovernorateWest of Iraq. Community Health Equity Research & Policy . 2021;42(3):253–6. https://doi.org/10.1177/0272684X20985708
Altaha lama H. The Missed symptoms of behjet’s disease. JFacMed Baghdad. 2021;63(1):13–7. https://iqjmc.uobaghdad.edu.iq/index.php/19JFacMedBaghdad36/article/view/1818
Al-Bazaz Na, MH Radhi Nj. Depression status in relation to dental caries and salivary C-Reactive Protein among 17 years old secondary school female in Baghdad City/Iraq. Journal of Baghdad College of Dentistry. 2021 15;33(1):6–11. https://doi.org/10.26477/jbcd.v33i1.2921
Khiala Hs, Diab Bs. Depression status in relation to caries experience and salivary physiochemical characteristics among 15 years old students in Al-Swera city at Wassit Governorate-Iraq. Journal of Baghdad College of Dentistry . 2015 ;27(2):158–62. https://jbcd.uobaghdad.edu.iq/index.php/jbcd/article/view/729
Sánchez J, Conejero C, Conejero R. Recurrent Aphthous Stomatitis. Actas DermoSifiliográficas (English Edition). 2020;111(6):471–80. https://www.sciencedirect.com/science/article/pii/S1578219020301724
Lau Cb, Smith Gp. Recurrent aphthous stomatitis: A comprehensive review and recommendations on therapeutic options. Dermatologic Therapy . 2022;35(6):e15500. https://doi.org/10.1111/dth.15500
Rivera C. Essentials of recurrent aphthous stomatitis (Review). Biomedical Reports. 2019;80(1). https://doi.org/10.3892/br.2019.1221
Bilodeau Ea, Lalla Rv. Recurrent oral ulceration: Etiology, classification, management, and diagnostic algorithm. Periodontology 2000. 2019;80(1):49–60. https://doi.org/10.1111/prd.12262
Klein B, Thoppay, Jaisri R, Scott, Ciarrocca K. Burning mouth syndrome. Dermatologic Clinics. 2020;38(4):477–83. https://doi.org/10.1016/j.det.2020.05.008
Adamo D, Spagnuolo G. Burning Mouth Syndrome: An Overview and Future Perspectives. International Journal of Environmental Research and Public Health. 2023;20(1). https://doi.org/10.3390/ijerph20010682
Kim Jy, Kim Ys, Ko I, Kim Dk. Association Between Burning Mouth Syndrome and the Development of Depression, Anxiety, Dementia, and Parkinson Disease. JAMA Otolaryngology–Head & Neck Surgery. 2020 Jun 1;146(6):561. https://doi.org/10.1001/jamaoto.2020.0526
Orliaguet M, Misery L. Neuropathic and Psychogenic Components of Burning Mouth Syndrome: A Systematic Review. Biomolecules. 2021;11(8). https://doi.org/10.3390/biom11081237
Teruel A, Patel S. Burning mouth syndrome: a review of etiology, diagnosis, and management. General dentistry. 2019;67(2):24–9. http://europepmc.org/abstract/MED/30875303
Tan Hl, Renton T. Burning mouth syndrome: An update. Cephalalgia Reports . 2020;3:2515816320970143. https://doi.org/10.1177/2515816320970143
Zheng Lw, Rezazadeh F, Farahmand F, Hosseinpour H, Shahriarirad R, Sabet, Amirhasan. The Association between Emotional Stress, Sleep Disturbance, Depression, and Burning Mouth Syndrome. BioMed Research International. 2021;2021:5555316. https://doi.org/10.1155/2021/5555316
Wrobel Bb, Leopold Da. Clinical assessment of patients with smell and taste disorders. Otolaryngologic Clinics of North America. 2004;37(6):1127–42. https://doi.org/10.1016/j.otc.2004.06.010
Wrobel Bb, Leopold Da. Smell and taste disorders. Facial Plastic Surgery Clinics of North America. 2004;12(4):459–68. https://doi.org/10.1016/j.fsc.2004.04.006
Boyce Jm. Effects of ageing on smell and taste. PMJ. 2006 ;82(966):239–41.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2579627/
Zhang Y, Chen Y, Chen J. The starch hydrolysis and aroma retention caused by salivary αamylase during oral processing of food. Current Opinion in Food Science [Internet]. 2022;43:237–45. https://www.sciencedirect.com/science/article/pii/S2214799321001600
Fatima S, Rehman A, Shah K, Kamran M, Mashal S, Rustam S, et al. Composition and function of saliva: A review. World J Pharm Pharm Sci. 2020;9(6):1552–67. https://www.wjpps.com/Wjpps_controller/abstract_id/12478
Ali N, Nater Um. Salivary AlphaAmylase as a Biomarker of Stress in Behavioral Medicine. International Journal of Behavioral Medicine. 2020;27(3):337–42. https://doi.org/10.1007/s1252901909843x
Wadsworth ME, Broderick AV, Loughlin‐Presnal JE, Bendezu JJ, Joos CM, Ahlkvist, Jarl A, et al. Co‐activation of SAM and HPA responses to acute stress: A review of the literature and test of differential associations with preadolescents’ internalizing and externalizing. Developmental psychobiology. 2019;61(7):1079–93. https://doi.org/10.1002/dev.21866
Khalid A, Zhang Q, Wang W, Ghaffari As, Pan F. The relationship between procrastination, perceived stress, saliva alphaamylase level and parenting styles in Chinese first year medical students. Psychology Research and Behavior Management. 2019;12:489–98. https://www.tandfonline.com/doi/abs/10.2147/PRBM.S207430
Walther L, Känel von, Zuccarellahackl C, Wirtz PH. Hyperreactivity of Salivary AlphaAmylase to Acute Psychosocial Stress and Norepinephrine Infusion in Essential Hypertension. Biomedicines. 2022;10(7). https://doi.org/10.3390/biomedicines10071762
.Morita K, Kimura H, Tsuka H, Nishio F, Yoshida M, Tsuga K. Association between salivary alphaamylase and subjective and objective oral parafunctions in communitydwelling elderly individuals. Journal of Dental Sciences [Internet]. 2020;15(3):310–4. Available from: https://www.sciencedirect.com/science/article/pii/S1991790220300866
Garrett Jr, Ekström J, Anderson L. Effects of autonomic nerve stimulations on salivary parenchyma and protein secretion. Neural mechanisms of salivary gland secretion [Internet]. 1999;11:59–79. https://www.karger.com/Article/Pdf/61112
Hensten A, Jacobsen N. Salivary alpha amylase as a stress biomarker. OSP J Dent Sci. 2019;1(1):1–6. https://www.ospublishers.com/pdf/JDS-1-103.pdf
Chi AC, Neville BW, Krayer JW, Gonsalves WC. Oral manifestations of systemic disease. American family physician. 2010 1;82(11):1381-8. PMID: 21121523
Meurman J, Basconesmartinez A. Oral Infections and Systemic HealthMore than Just Links to Cardiovascular Diseases. Oral health & preventive dentistry. 2021;19(1):441–8. DOI: 10.3290/j.ohpd.b1993965
Nazir MA, Izhar F, Akhtar K, Almas K. Dentists’ awareness about the link between oral and systemic health. Journal of Family & Community Medicine. 2019 Sep 1;26(3):206–12. https://pubmed.ncbi.nlm.nih.gov/31572052/
Esguep A. Association between psychological disorders and the presence of Oral lichen planus, Burning mouth syndrome and Recurrent aphthous stomatitis. Medicina oral: organooficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal. 2004;9(1):1–7. PMID: 14704611
De Porrascarrique, Teresa, Gonzálezmoles Má, Warnakulasuriya S, Ramosgarcía P. Depression, anxiety, and stress in oral lichen planus: a systematic review and metaanalysis. Clinical Oral Investigations. 2022;26(2):1391–408. https://doi.org/10.1007/s00784021041140
Dibello V, Ballini A, Lozupone M, Custodero C, Cantore S, Sardone R, et al. Exploring the Association of Burning Mouth Syndrome with Depressive and Anxiety Disorders in MiddleAged and Older Adults: A Systematic Review. Journal of Personalized Medicine. 2023;13(6). https://doi.org/10.3390/jpm13061014
Kim J, Kim YS, Ko I, Kim D. Association Between Burning Mouth Syndrome and the Development of Depression, Anxiety, Dementia, and Parkinson Disease. JAMA Otolaryngol Head Neck Surg . 2020 ;146(6):561–9. https://doi.org/10.1001/jamaoto.2020.0526
Rivera C. Essentials of recurrent aphthous stomatitis. Biomedical reports. 2019 ;11(2):47-50. https://doi.org/10.3892/br.2019.1221
Hariyani N, Bramantoro T, Nair R, Singh A, Sengupta K. Depression symptoms and recurrent aphthous stomatitis—Evidence from a populationbased study in Indonesia. Oral Dis [Internet]. 2020 [cited 2023 Jul 22];26(5):948–54. https://doi.org/10.1111/odi.13303
Wiriyakijja P, Porter S, Fedele S, Hodgson T, McMillan R, Shephard M, et al. Validation of the HADS and PSS10 and a crosssectional study of psychological status in patients with recurrent aphthous stomatitis. J Oral Pathol Med . 2020;49(3):260–70. https://doi.org/10.1111/jop.12991
Darjani A, Joukar F, Naghipour M, Asgharnezhad M, MansourGhanaei F. Lifetime prevalence of recurrent aphthous stomatitis and its related factors in Northern Iranian population: The PERSIAN Guilan Cohort Study. Clinical Oral Investigations . 2021;25(2):711–8. https://doi.org/10.1007/s0078402003611y
Wang Z, Cao H, Xiong J, Lu Y, Deng Y, Nan H, et al. Recent advances in the aetiology of recurrent aphthous stomatitis (RAS). Postgrad Med J. 2022 ;98(1155):57–66. Available from: https://doi.org/10.1136/postgradmedj2020139421
Schiavone V, Adamo D, Ventrella G, Morlino M, De Notaris EB, Ravel MG, et al. Anxiety, Depression, and Pain in Burning Mouth Syndrome: First Chicken or Egg? Headache: The Journal of Head and Face Pain. 2012 May 18;52(6):1019–25. https://doi.org/10.1111/j.1526-4610.2012.02171.x
Richter I, Vidas I, Turčinović P. Relationship of psychological characteristics and oral diseases with possible psychosomatic aetiology. Acta stomatologica Croatica: International journal of oral sciences and dental medicine. 2003;37(1):27–34. https://hrcak.srce.hr/file/4275
Kao C, Kao C, Ma KS, Huang T. The association of burning mouth syndrome with depression. Journal of Dental Sciences. 2023;18(1):456. https://doi.org/10.1016/j.jds.2022.08.028
Galli F, Pravettoni G. Burning Mouth Syndrome—Opening the Door to a Psychosomatic Approach in the Era of PatientCentered Medicine. JAMA Otolaryngol Head Neck Surg . 2020 ;146(6):569–70. https://doi.org/10.1001/jamaoto.2020.0524
Fawzi OF, Al-Aswad FD. Oral manifestations, biochemical, and IL-6 analysis of saliva in major depressive disorder patients under treatment. Journal of Baghdad College of Dentistry . 2013;25(2):89–93. https://jbcd.uobaghdad.edu.iq/index.php/jbcd/article/view/234
Klein B, Thoppay, Jaisri R, Scott, Ciarrocca K. Burning mouth syndrome. Dermatologic Clinics. 2020;38(4):477–83. https://doi.org/10.1016/j.det.2020.05.008
Imamura Y, Shinozaki T, OkadaOgawa A, Noma N, Shinoda M, Iwata K, et al. An updated review on pathophysiology and management of burning mouth syndrome with endocrinological, psychological and neuropathic perspectives. J Oral Rehabil . 2019;46(6):574–87. https://doi.org/10.1111/joor.12795
Tan HL, Renton T. Burning mouth syndrome: An update. Cephalalgia Reports . 2020;3:2515816320970143. https://doi.org/10.1177/2515816320970143
Dror C, Braw Y, Maoz H, Mendlovic S, Granovsky Y, Bloch Y, et al. Pain perception and modulation profiles in patients suffering from unipolar and bipolar depression. Journal of Affective Disorders Reports. 2023;12:100496. https://www.sciencedirect.com/science/article/pii/S2666915323000343
Miller SM, Naylor GJ. Unpleasant taste — a neglected symptom in depression. Journal of Affective Disorders. 1989;17(3):291–3. https://doi.org/10.1016/0165-0327(89)90013-X
Burges Watson DL, Campbell M, Hopkins C, Smith B, Kelly C, Deary V. Altered smell and taste: Anosmia, parosmia and the impact of long Covid-19. Andaloro C, editor. PLOS ONE. 2021;16(9):e0256998. https://doi.org/10.1371/journal.pone.0256998
Hur K, Choi JS, Zheng M, Shen J, Wrobel B. Association of alterations in smell and taste with depression in older adults. Laryngoscope Investigative Otolaryngology . 2018 ;3(2):94–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5915822/
Steiner JE, Rosenthalzifroni A, Edelstein EL. Taste perception in depressive illness. Israel Annals of Psychiatry & Related Disciplines. 1969;7:223–32. PMID: 5274360
Gelder M, Harrison P, Cowen P. Symptoms and signs of psychiatric disorders. Shorter textbook of psychiatry 5th edition New York: Oxford. 2008;1–20. https://doi.org/10.1093/med/9780198747437.003.0001
Kim D, Chung S, Lee Sh, Koo Jh, Lee J, Jahng, Jeong Won. Decreased expression of 5HT1A in the circumvallate taste cells in an animal model of depression. Archives of oral biology. 2017;76:42–7. https://doi.org/10.1016/j.archoralbio.2017.01.005
Tanra, Andi Jayalangkara, Madeali H, Sanusi M, Syamsuddin S, Lisal St. Salivary Alphaamylase Enzyme and Salivary Cortisol Level in Depression after Treatment with Fluoxetine. Open Access Maced J Med Sci. 2021;9(T3):305310.https://oamjms.eu/index.php/mjms/article/view/6347
Stegeren Van, Rohleder N, Everaerd W, Wolf Ot. Salivary alpha amylase as marker for adrenergic activity during stress: Effect of betablockade. Psychoneuroendocrinology. 2006;31(1):137–41. https://www.sciencedirect.com/science/article/pii/S0306453005001289
Tanaka Y, Ishitobi Y, Maruyama Y, Kawano A, Ando T, Okamoto S, et al. Salivary alphaamylase and cortisol responsiveness following electrical stimulation stress in major depressive disorder patients. Progress in NeuroPsychopharmacology and Biological Psychiatry . 2012;36(2):220–4. https://www.sciencedirect.com/science/article/pii/S0278584611002880
Stegeren van, Rohleder N, Everaerd W, Wolf Ot. Salivary alpha amylase as marker for adrenergic activity during stress: Effect of betablockade. Psychoneuroendocrinology . 2006;31(1):137–41. https://www.sciencedirect.com/science/article/pii/S0306453005001289
Ishitobi Y, Akiyoshi J, Tanaka Y, Ando T, Okamoto S, Kanehisa M, et al. Elevated salivary αamylase and cortisol levels in unremitted and remitted depressed patients. International journal of psychiatry in clinical practice. 2010;14(4):268–73. https://doi.org/10.3109/13651501.2010.500737
Busch L, Sterinborda L, Borda E. An Overview of Autonomic Regulation of Parotid Gland Activity: Influence of Orchiectomy. Cells Tissues Organs. 2006;182(34):117–28. https://www.karger.com/DOI/10.1159/000093962
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Ameer AlThabhawee, Taghreed F Zaidan, Mohammed Ali

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


