The Role of Small Dense Low-Density Lipoprotein in Diabetic Retinopathy
DOI:
https://doi.org/10.32007/jfacmedbaghdad2942Keywords:
Diabetes mellitus, Non-proliferative diabetic retinopathy, proliferative diabetic retinopathy , Small dense low density lipoprotein, TriglycerideAbstract
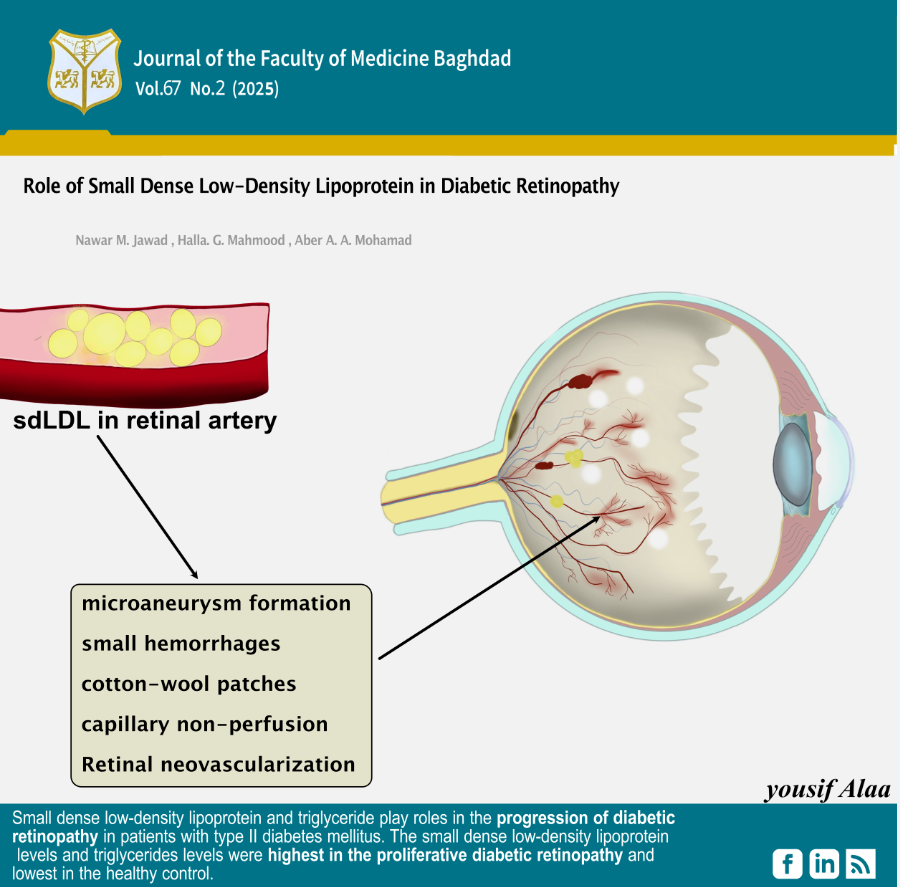
Background: Diabetic retinopathy is the primary ocular outcome of diabetes mellitus, a serious disease that significantly impacts global health. Microvascular complications arise from damage to small blood vessels, including retinopathy, nephropathy, cardiomyopathy, and neuropathy. Inconsistent findings exist in epidemiological research that specifically examines lipid levels and diabetic retinopathy. The small, dense Low-Density Lipoprotein particles are a specific subset of Low-Density Lipoprotein that possesses several pro-atherogenic characteristics.
Objectives: to evaluate the usefulness of serum small dense low-density lipoprotein level as a biomarker for predicting patients with type II diabetes mellitus who suffer from proliferative and non-proliferative diabetic retinopathy.
Methods: The study involved 160 individuals divided into four groups: 40 patients with non-proliferative diabetic retinopathy, 40 patients with proliferative diabetic retinopathy, 40 controlled diabetic patients without diabetic retinopathy, and 40 healthy controls. Student’s t-test and ANOVA were employed to compare the means between the groups.
Results: The study revealed that small dense low-density lipoprotein levels in the proliferative diabetic retinopathy group were significantly higher than those in the non-proliferative diabetic retinopathy, diabetic without retinopathy, and healthy control groups. The mean and standard deviation in patients with proliferative diabetic retinopathy were 4.70±1.96 µmol/L, in non-proliferative diabetic retinopathy, it was 3.00±0.90 µmol/L, in diabetic patients without retinopathy, it was 2.51±0.53 µmol/L, and in healthy controls, it was 2.45± 0.48 µmol/L.
Conclusion: Small, dense, low-density lipoprotein and triglycerides play roles in the progression of diabetic retinopathy in patients with type II diabetes mellitus. The small, dense, low-density lipoprotein and triglyceride levels were highest in the proliferative diabetic retinopathy and lowest in the healthy control.
Received: Oct. 2024
Revised: Feb. 2025
Accepted: Mar. 2025
Published Online: April 2025
Published: July 2025
References
1. Antonetti DA, Silva PS, Stitt AW. Current understanding of the molecular and cellular pathology of diabetic retinopathy. Nature Reviews Endocrinology. 2021;17:195-206. https://doi.org/10.1038/s41574-020-00451-4.
2. Kropp M, Golubnitschaja O, Mazurakova A, et al. Diabetic retinopathy as the leading cause of blindness and early predictor of cascading complications—risks and mitigation. EPMA Journal. 2023;14:21-42. https://doi.org/10.1007/s13167-023-00314-
3. Zhou J, Chen B. Retinal cell damage in diabetic retinopathy. Cells. 2023;12(9):1342. https://doi.org/10.3390/cells12091342.
4. Albadr A, Haddad NS. Pancreatic Stone Protein/regenerating Protein (PSP/reg) as a Biochemical Marker for prediction of Microvascular Complications of Type 2 Diabetes Mellitus. KCMJ. 2023;19(2):196-201. https://doi.org/10.47723/kcmj.v19i2.966.
5. Szczechla M, Balewska A, Naskręt D, Zozulińska-Ziółkiewicz D, Uruska A. Molecular Changes in Cells of Patients with Type 2 Diabetes Mellitus Depending on Changes in Glycemia Level in the Context of Lifestyle—An Overview of the Latest Scientific Discoveries. CIMBiology. 2023;45(3):1961-81. https://doi.org/10.3390/cimb45030126.
6. AlKenany Q, Rasheed MK, AlKazraj KA. The Predictive Role of Osteopontin Level in Patients with Type 2 Diabetes Mellitus without Fatty Liver Disease. JFacMedBaghdad. 2024;66(1):93-8. https://doi.org/10.32007/jfacmedbagdad.6612182
7. Al-Yassin HD. Correlation of Serum levels of Chromium, Copper, and Manganese with the Glucose levels in Type 2 Diabetes Mellitus in Iraq. JFacMedBaghdad. 2023;65(4). https://doi.org/10.32007/jfacmedbagdad.2126
8. Taha BE, Majeed MJ. Estimation of Insulin Resistance in Obese Adults in Baghdad. JFacMed Baghdad. 2023;65(4). https://doi.org/10.32007/jfacmedbagdad.2118.
9. Liu Z, Shao M, Ren J, Qiu Y, Li S, Cao W. Association between increased lipid profiles and risk of diabetic retinopathy in a population-based case-control study. JIR. 2022;15:3433-46. https://doi.org/10.2147/JIR.S361613.
10. Julve J, Rossell J, Correig E, et al. Predictive value of the advanced lipoprotein profile and glycated proteins on diabetic retinopathy. Nutrients. 2022;14(19):3932. https://doi.org/10.3390/nu14193932.
11. Hirano T, Hayashi T, Sugita H, et al. Prospective randomized comparative study of the effect of pemafibrate add‐on or double statin dose on small dense low‐density lipoprotein‐cholesterol in patients with type 2 diabetes and hypertriglyceridemia on statin therapy. J Diabetes Investig. 2023;14(12):1401-11. https://doi.org/10.1111/jdi.14076
12. Sun C, Chen Q, Zhang X, et al. Peripheral Neuropathy Is Associated With High Serum Levels of Small Dense Low-density Lipoprotein-cholesterol in Patients With Type 2 Diabetes Mellitus. 2021.
13. Otrante A, Bounafaa A, Berrougui H, Essamadi A-K, Nguyen M, Fülöp T, et al. Small Dense LDL Level and LDL/HDL Distribution in Acute Coronary Syndrome Patients. Biomedicines. 2023;11(4):1198. https://doi.org/10.3390/biomedicines11041198
14. Płaczkowska S, Sołkiewicz K, Bednarz-Misa I, Kratz EM. Atherogenic plasma index or non-high-density lipoproteins as markers best reflecting age-related high concentrations of small dense low-density lipoproteins. IJMS. 2022;23(9):5089. https://doi.org/10.3390/ijms23095089
15. Nakayama A, Morita H, Sato T, et al. Small dense low-density lipoprotein cholesterol is a potential marker for predicting laser treatment for retinopathy in diabetic patients. JAT. 2022;29(5):678-91. https://doi.org/10.5551/jat.62889
16. Atchison E, Barkmeier A. The role of systemic risk factors in diabetic retinopathy. Current Ophthalmology Reports. 2016;4:84-9. https://doi.org/10.1007/s40135-016-0098-8.
17. Soedarman S, Kurnia KH, Prasetya ADB, Sasongko MB. Cholesterols, apolipoproteins, and their associations with the presence and severity of diabetic retinopathy: a systematic review. Vision. 2022;6(4):77. https://doi.org/10.3390/vision6040077
18.Bryl A, Mrugacz M, Falkowski M, Zorena K. The Effect of Hyperlipidemia on the Course of Diabetic Retinopathy—Literature Review. JCM. 2022;11(10):2761. https://doi.org/10.3390/jcm11102761
19. Hukportie DN, Li FR, Zhou R, et al. Lipid variability and risk of microvascular complications in Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: A post hoc analysis. J Diabetes. 2022;14(6):365-76. https://doi.org/10.1111/1753-0407.13273
20. Li Z, Yuan Y, Qi Q, Wang Q, Feng L. Relationship between dyslipidemia and diabetic retinopathy in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Syst Rev. 2023; 12:148. https://doi.org/10.1186/s13643-023-02321-2
21. Romero-Aroca P, Verges R, Pascual-Fontanilles J, et al. Effect of Lipids on Diabetic Retinopathy in a Large Cohort of Diabetic Patients after 10 Years of Follow-Up. JCM. 2023;12(20):6674. https://doi.org/10.3390/jcm12206674
22. Chou Y, Ma J, Su X, Zhong Y. Emerging insights into the relationship between hyperlipidemia and the risk of diabetic retinopathy. Lipids Health Dis. 2020; 19:241. https://doi.org/10.1186/s12944-020-01415-3
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Nawar M. Jawad, Halla G. Mahmood, Abeer A. Mohammed

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


