Comparison of ََQuality of Life and Treatment Satisfaction among Sample of Iraqi Patients Using Anticoagulant Therapy (Warfarin or Non-Vitamin K Antagonist Oral Anticoagulants)
DOI:
https://doi.org/10.32007/jfacmedbaghdad.6632267Keywords:
Warfarin, NOAC, Quality of life, Satisfaction, Iraqi patientsAbstract
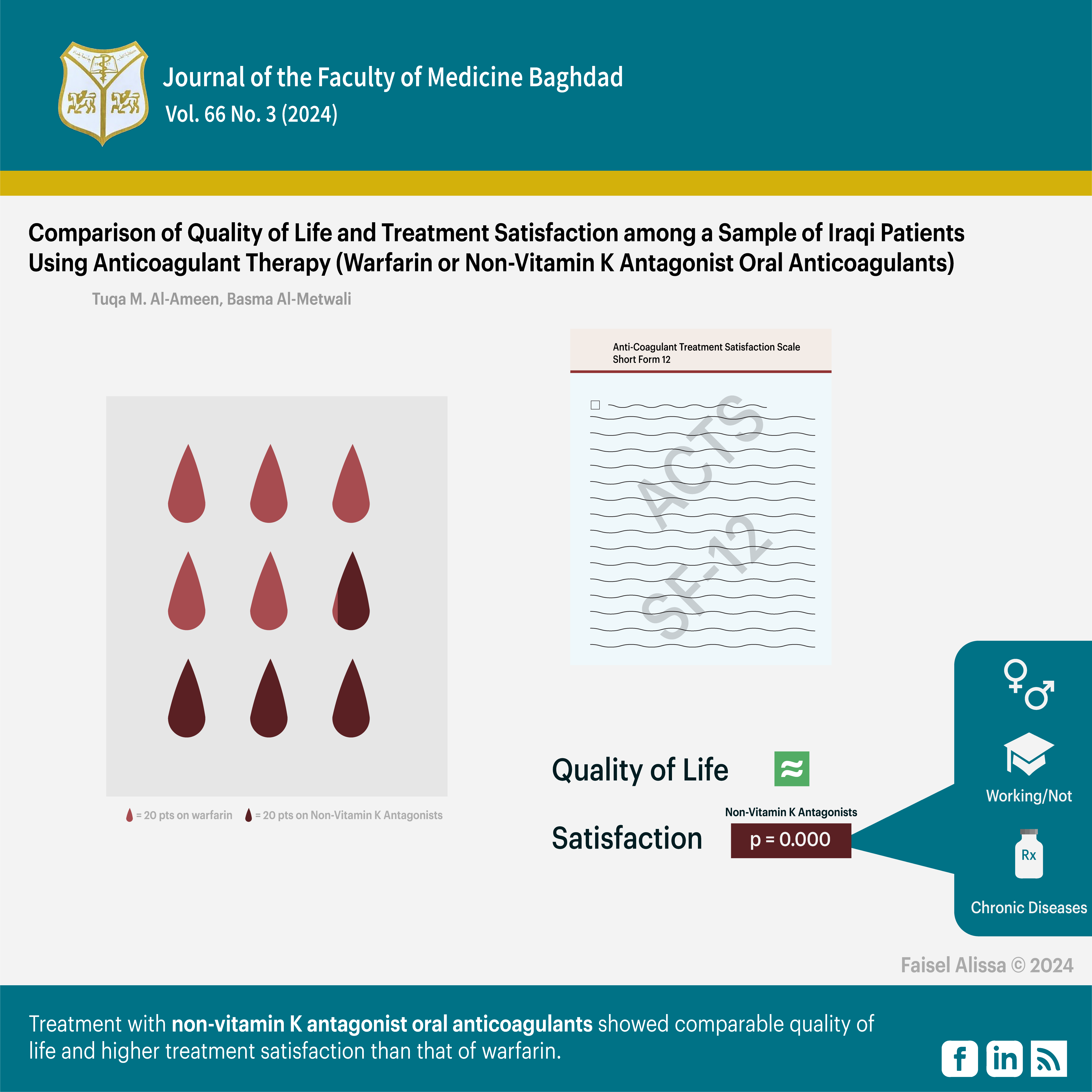
Background: Oral anticoagulation medication, warfarin and non-vitamin k antagonist oral anticoagulants (NOAC) may require long term use which may affect patients’ satisfaction with their treatment and their quality of life (QOL).
Objective: To compare the quality of life and treatment satisfaction among groups of patients using different anticoagulant therapies (warfarin and NOAC).
Patients and methods: A cross-sectional study was performed at Ibn Al-Bitar Hospital for cardiac surgery in Baghdad in the period between December 2022 to May 2023. The study population included a convenient sample of patients receiving either warfarin or non-vitamin k antagonist oral anticoagulants treatment. The Arabic version of the short form 12 (SF-12) questionnaire and the Anti-Coagulant Treatment Satisfaction Scale (ACTS) questionnaire were used to assess the quality of life and satisfaction with treatment respectively.
Results: The study included 181 patients in total. The mean physical and mental quality of life scores for study participants were 42.3±9.92 and 52.6±10.36 respectively. There was no significant difference in the QOL between patients taking warfarin and those on non-vitamin k antagonist oral anticoagulants treatment. The mean total satisfaction score was 65.4±6.73. Patients receiving non-vitamin k antagonist oral anticoagulants had significantly higher satisfaction compared to those receiving warfarin (P=0.000). The physical score correlated significantly with gender, educational level, employment status, number of chronic medications and number of chronic diseases. The total satisfaction score correlated significantly with gender, number of chronic medications, number of side effects and duration of anticoagulation. There was a significant correlation between the QOL and treatment satisfaction (P=0.000).
Conclusion: Treatment with non-vitamin k antagonist oral anticoagulants showed comparable QOL and higher treatment satisfaction than that of warfarin. Better treatment satisfaction can improve patients’ QOL which may ultimately enhance their adherence to treatment.
Received: Dec. 2023
Revised: April. 2024
Accepted: May. 2024
Downloads
References
Ho KH, van Hove M, Leng G. Trends in anticoagulant prescribing: a review of local policies in English primary care. BMC Health Services Research. 2020 Apr 3;20(1): 279. https://doi.org/10.1186/s12913-020-5058-1.
Sharma RK. Recent Advancements in Oral Anticoagulants: A Systematic Review. Nep. Med. J. 2022 Jun. 30;5(1):552-8. https://doi.org/10.3126/nmj.v5i1.44920.
Cohen A, Dobromirski M. The use of rivaroxaban for short- and long-term treatment of venous thromboembolism. Thrombosis and Haemostasis. 2012;107(6):1035–43. https://doi.org/10.1160/TH11-12-0859.
4. Lee SR, Choi EK, Kwon S, Jung JH, Han KD, Cha MJ, et al. Effectiveness and Safety of Direct Oral Anticoagulants in Relation to Temporal Changes in Their Use. Circulation Cardiovascular Quality and Outcomes. 2020 Mar 1;13(3):e005894. https://doi.org/10.1161/CIRCOUTCOMES.119.005894.
5. Bratsos S. Pharmacokinetic Properties of Rivaroxaban in Healthy Human Subjects. Cureus. 2019 Aug 25;11(8). https://doi.org/10.7759/cureus.5484 .
Königsbrügge O, Ay C. Atrial fibrillation in patients with end‐stage renal disease on hemodialysis: Magnitude of the problem and new approach to oral anticoagulation. Research and Practice in Thrombosis and Haemostasis. 2019 Aug 18;3(4):578–88. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6781927/.
7. Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood advances. 2020 Oct 13;4(19):4693-4738. https://doi.org/10.1182/bloodadvances.2020001830.
The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychological Medicine. 1998 May;28(3):551–8. https://doi.org/10.1017/s0033291798006667.
Loge JH, Kaasa S. Quality of life and patient-reported outcome measures. Oxford University Press eBooks. 2021 Aug 1;1318–1327. https://academic.oup.com/book/40580/chapter-abstract/348141068?redirectedFrom=fulltext&login=false.
Iqbal MS, Muthanna FMS, Kassab YW, Hassali MA, Al-Saikhan FI, Iqbal MZ, et al. Determinants of health-related quality of life among warfarin patients in Pakistan. PLOS ONE. 2020;15(6):e0234734. https://doi.org/10.1371/journal.pone.0234734.
Keita I, Aubin-Auger I, Lalanne C, Aubert JP, Chassany O, Duracinsky M, et al. Assessment of quality of life, satisfaction with anticoagulation therapy, and adherence to treatment in patients receiving long-course vitamin K antagonists or direct oral anticoagulants for venous thromboembolism. Patient Preference and Adherence. 2017 Sep 25;11:1625–1634. https://doi.org/10.2147/PPA.S131157 .
12. Weaver M, Patrick DL, Markson LE, Martin D, Frederic I, Berger M. Issues in the measurement of satisfaction with treatment. The American Journal of Managed Care. 1997;3(4):579–94. https://doi.org/10.1007/s40271-024-00702-w.
Swiatoniowska-Lonc N, Tanski W, Polanski J, Jankowska-Polanska B. Treatment satisfaction and pharmacological adherence in patients with chronic diseases. European Journal of Cardiovascular Nursing. 2022 Jul 1;21(Supplement_1). https://doi.org/10.1093/eurjcn/zvac060.067
Suárez Fernández C, Castilla-Guerra L, Cantero-Hinojosa J, Suriñach JM, Acosta de Bilbao F, Tamarit JJ, et al. Satisfaction with oral anticoagulants in patients with atrial fibrillation. Patient Preference and Adherence. 2018 Feb;Volume 12:267–274. https://doi.org/10.2147/PPA.S152109 .
15. Benzimra M, Bonnamour B, Duracinsky M, Lalanne C, Aubert JP, Chassany O, et al. Real-life experience of quality of life, treatment satisfaction, and adherence in patients receiving oral anticoagulants for atrial fibrillation. Patient Preference and Adherence. 2018;12:79-87. https://doi.org/10.2147/PPA.S131158.
Ng DLC, Gan GG, Chai CS, Chee KH, Tan KL, Tan SB, et al. Comparing quality of life and treatment satisfaction between patients on warfarin and direct oral anticoagulants: a cross-sectional study. Patient Preference and Adherence. 2019; 13:1363–1373. https://doi.org/10.2147/PPA.S204246.
17. Najaf HN, Kadhim DJ. Health-related quality of life among a sample of chronic hepatitis B patients in AL-Najaf Province/Iraq. Iraqi Journal of Pharmaceutical Sciences. 2020;29(1):33-40. https://doi.org/10.31351/vol29iss1pp33-40.
A. Sabry S, J. Ibrahem M, Jabarah MA. Relationship of the quality of life in capecitabine-treated colorectal cancer patients to sociodemographic characteristics and drug-related adverse effects. JFacMedBagdad. 2022;64(3):175-82. https://iqjmc.uobaghdad.edu.iq/index.php/19JFacMedBaghdad36/article/view/1970.
Ghayadh AA, Naji AB. Treatment Adherence and its Association to Quality of Life among Patients with Hypertension. Pakistan Heart Journal. 2023 May 16;56(2):44–9 .
H. Qasim T, J. Ibraheem M, Jabarah MA-H. Impact of sociodemographic characteristics and drug-related side effects on quality of life of patients with hepatocellular carcinoma receiving sorafenib treatment in Iraqi hospitals. JFacMedBagdad. 2023 Jan. 13. 27;64(4):286-91. https://iqjmc.uobaghdad.edu.iq/index.php/19JFacMedBaghdad36/article/view/2009.
21. Abdul-Hameed AK, Abd RI, Handel AS. Assessing the Knowledge of Patients with Atrial Fibrillation Using Oral Anticoagulants Medications. Pakistan Journal of Medical and Health Sciences. 2022 Mar 31;16(3):1008–10. https://doi.org/10.53350/pjmhs221631008 .
22. Al-Shehri AH, Taha AZ, Bahnassy AA, Salah M. Health-related quality of life in type 2 diabetic patients. Annals of Saudi Medicine. 2008 Sep;28(5):352–60. https://doi.org/10.5144/0256-4947.2008.352 .
Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology. 1998 Nov 1;51(11):1171–8. https://doi.org/10.1016/s0895-4356(98)00109-7.
Ware John E et al. Sf-12: How to Score the Sf-12 Physical and Mental Health Summary Scales. 3. ed. Quality Metric Inc.; Health Assessment Lab 1998.
Shilbayeh SAR, Ibrahim AA. The anti-clot treatment scale (ACTS): validation of the translated Arabic version among patients undergoing warfarin therapy in Saudi Arabia. Health and Quality of Life Outcomes. 2020 Jul 6;18(1):215. https://doi.org/10.1186/s12955-020-01471-4.
Cano SJ, Lamping DL, Bamber L, Smith S. The Anti-Clot Treatment Scale (ACTS) in clinical trials: cross-cultural validation in venous thromboembolism patients. Health and Quality of Life Outcomes. 2012;10(1):120. https://doi.org/10.1186/1477-7525-10-120 .
Fang MC, Gob AS, Prasad PA, Zhou HX, Parks AL, Fan D, et al. Health-related quality of life associated with warfarin and direct oral anticoagulants in venous thromboembolism. Thrombosis Research. 2022;216:97-102. https://doi.org/10.1016/j.thromres.2022.06.008 .
Bavalia R, Bistervels IM, Boersma WG, Quere I, Brisot D, Falvo N, et al. Quality of life in patients with pulmonary embolism treated with edoxaban versus warfarin. Research and Practice in Thrombosis and Haemostasis. 2021 Jul;5(5):e12566. https://doi.org/10.1002/rth2.12566 .
Sulaiman I & Kadhim D. Qََََuality of life of patients with end stage renal disease on haemodialysis comparing to patients underwent kidneys transplantation in Iraq. Iraqi New Medical Journal. 2019 Jan;5(9).
Kareem AH, Kadhim DJ. Health-Related Quality of Life in a Sample of Chronic Obstructive Pulmonary Disease Patients in AL-Diwanyia Province /Iraq. Iraqi Journal of Pharmaceutical Sciences [Internet]. 2020 Dec 1;29(2):169-175. DOI: https://doi.org/10.31351/vol29iss2pp169-175.
Varaklioti A, Nika S, Papachronis A, Chanos A, Gkotsi S, Pyrpyri T, et al. PB2360: Quality of life and treatment satisfaction among patients under long-term anticoagulant therapy with vitamin k antagonists. HemaSphere. 2022 Jun 1; 6(Suppl): 2229-2230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9429850.
Gorial FI, Jabbar MA. Impact of disease activity on health-related quality of life in patients with Behçet’s disease: A cross-sectional study. Annals of Medicine and Surgery. 2020;54:43–46. https://doi.org/10.1016/j.amsu.2020.03.010 .
Abdulridha SH, Kadhim DJ, Abdul Razzak SA. Assessment of Quality of Life in a Sample of Iraqi Patients with Psoriasis. Iraqi Journal of Pharmaceutical Sciences. 2020 Dec 30;29(2):161–168. https://doi.org/10.31351/vol29iss2pp161-168.
Faiq MK, Kadhim DJ, Gorial FI. Assessing quality of life among sample of Iraqi patients with rheumatoid arthritis. International Journal of Research in Pharmaceutical Sciences. 2019;10(4): 2856-2863.https://doi.org/10.26452/ijrps.v10i4.1564
Iqbal MS, Kassab YW, Al-Saikhan FI, Almalki ZS, Haseeb A, Iqbal MZ, et al. Assessing quality of life using WHOQOL-BREF: A cross-sectional insight among patients on warfarin in Malaysia. Saudi Pharmaceutical Journal. 2020 Aug;28(8):936–942. https://doi.org/10.1016/j.jsps.2020.06.014.
Chang YF, Yeh CM, Huang SL, Ho CC, Li RH, Wang WH, et al. Work Ability and Quality of Life in Patients with Work-Related Musculoskeletal Disorders. International Journal of Environmental Research and Public Health. 2020 May 9;17(9):3310. https://doi.org/10.1016/j.jsps.2020.06.014.
Perelman NL. Impact of comorbid pathology on the quality of life of patients with bronchial asthma. Bulletin Physiology and Pathology of Respiration. 2022 Jul 8;1(84):8–14.
https://doi.org/10.36604/1998-5029-2022-84-8-14
Mannan A, Akter KM, Akter F, Chy NUHA, Alam N, Pinky SD, et al. Association between comorbidity and health-related quality of life in a hypertensive population: a hospital-based study in Bangladesh. BMC Public Health. 2022 Jan 26;22:181. https://doi.org/10.1186/s12889-022-12562-w.
Fang MC, Go AS, Prasad PA, Hsu JW, Fan D, Portugal C, et al. Anticoagulant treatment satisfaction with warfarin and direct oral anticoagulants for venous thromboembolism. Journal of Thrombosis and Thrombolysis. 2021 Apr 8; 52(4):1101-1109. https://doi.org/ 10.1007/s11239-021-02437 –z.
Salmasi S, Adelakun A, Safari A, Kwan L, MacGillivray J, Andrade JG, et al. Satisfaction with Oral Anticoagulants Among Patients with Atrial Fibrillation: A Prospective Observational Study. CJC Open. 2021 Jun;3(11):1347–1356. https://doi.org/10.1016/j.cjco.2021.06.015 .
Ucar A, Arslan S. Perception of Treatment Satisfaction in Patients who Receive Warfarin Therapy in Turkey. International Journal of Caring Sciences. 2021;14:(1)–570=580. https://www.internationaljournalofcaringsciences.org/docs/60_ucar_original_14_1.pdf.
Akgün S, Tunç Karaman S, Özdemir S, Basat O. Evaluation of Oral Anticoagulant Usage Satisfaction in Home Care Patients Using Warfarin. Journal of Academic Research in Medicine. 2021 Apr 30;11(1):38–45. https://doi.org/10.4274/jarem.galenos.2021.3732.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Basma Z. Al-Metwali, Tuqa M. AL-Ameen

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


