The Role of Serum and Seminal Fluid Anti-Müllerian Hormone (AMH) in Differentiating Subtypes of Male Infertility.
DOI:
https://doi.org/10.32007/jfacmedbaghdad3131Keywords:
Anti-Müllerian Hormone, Asthenozoospermia, Plasma Seminal FluidAbstract
Background: Infertility is the inability to conceive after one year of unprotected intercourse, with male factors accounting for about 50% of cases. Anti-Müllerian hormone (AMH), a glycoprotein belonging to the Transforming growth factor beta family, is secreted from Sertoli cells and plays a key role in male sexual differentiation.
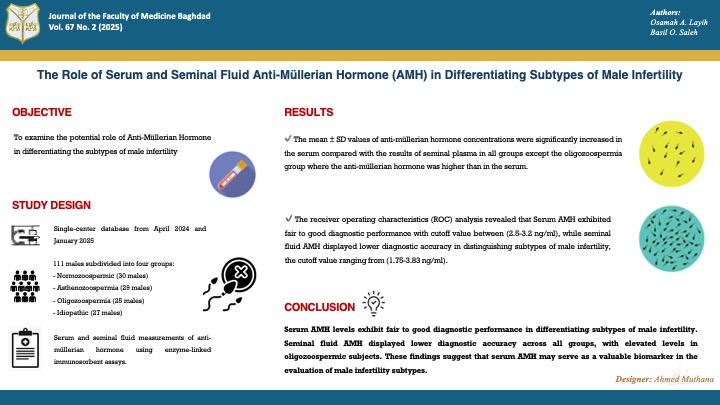
Objectives: To examine the potential role of Anti-Müllerian Hormone in differentiating the subtypes of male infertility.
Methods: This case-control study was done at the Infertility Center of Al-Batool Teaching Hospital in Diyala Governorate, Iraq, by the Department of Biochemistry / College of Medicine / University of Baghdad between April 2024 and January 2025. It included 111 males, aged 20-55 years. These subjects were subdivided into four groups based on seminal fluid analysis: The Normozoospermic group (30 males), who served as the control group; the Asthenozoospermia group (29 males); the oligozoospermia group (25 males); and the idiopathic (unexplained) infertility group (27 males). Investigations included serum and seminal fluid measurements of anti-müllerian hormone using enzyme-linked immunosorbent assays.
Results: The mean ±SD values of anti-müllerian hormone concentrations were significantly higher in the serum compared with the results of seminal plasma in all groups except the oligozoospermia group, where the AMH was higher than in the serum. The receiver operating characteristics (ROC) analysis revealed that Serum AMH exhibited fair to good diagnostic performance with cutoff value between (2.5-3.2 ng/ml), while seminal fluid AMH displayed lower diagnostic accuracy in distinguishing subtypes of male infertility, the cutoff value ranging from (1.75-3.83 ng/ml).
Conclusion: Serum AMH levels exhibit fair to good diagnostic performance in differentiating subtypes of male infertility. Seminal fluid AMH displayed lower diagnostic accuracy across all groups, with elevated levels in oligozoospermic subjects. These findings suggest that serum AMH may be a valuable biomarker in evaluating male infertility subtypes.
Received: March 2025
Revised: March 2025
Accepted: April 2025
Published Online: April 2025
Published: July 2025
References
1. Ghewade P, Vagha S, Ghewade B, Gadkari P. Role of Dietary Antioxidant Supplements in Male Infertility: A Review. Cureus. 2024;16(6). https://doi.org/10.7759/cureus.61951
2. Agarwal A, Baskaran S, Parekh N, Cho CL, Henkel R, Vij S, et al. Male infertility. The Lancet. 2021;397(10271):319-33. https://doi.org/10.1016/S0140-6736(20)32667-2
3. Alani GT, El Yaseen HD. Creatine kinase activity and malondialdehyde in the seminal plasma of normospermic infertile males. Journal of the Faculty of Medicine Baghdad. 2009;51(3):336-40.
https://doi.org/10.32007/jfacmedbagdad.5131146
4. Aziz ASA, Elyaseen HD. Kadhem HK. Correlation between MDA Level and Chitotriosidase-1 Activity in Seminal Fluid of Iraqi Infertile Males. Journal of the Faculty of Medicine Baghdad. 2024;66(4):479-86. https://doi.org/10.32007/jfacmedbaghdad.6642395
5. Pereira R, Sousa M. Morphological and molecular bases of male infertility: a closer look at sperm flagellum. Genes. 2023;14(2):383. https://doi.org/10.3390/genes14020383
6. Salman FS, Al-Qadhi HI, Al Kareem BA. N-acetyl cysteine's effect on semen parameters in a sample of Iraqi men with oligoasthenoteratozoospermia. Journal of the Faculty of Medicine Baghdad. 2022;64(3):170-4. https://doi.org/10.32007/jfacmedbagdad.6431938
7. Xu H, Zhang M, Zhang H, Alpadi K, Wang L, Li R, et al. Clinical Applications of Serum Anti-Müllerian Hormone Measurements in Both Males and Females: An Update. Innovation. 2021;2(1):100091. https://doi.org/10.1016/j.xinn.2021.100091
8. Josso N, Picard JY. Genetics of anti-Müllerian hormone and its signaling pathway. Best Practice & Research Clinical Endocrinology & Metabolism. 2022;36(1):101634. https://doi.org/10.1016/j.beem.2022.101634
9. Howard JA, Hart KN, Thompson TB. Molecular mechanisms of AMH signaling. Frontiers in Endocrinology. 2022;13:927824. https://doi.org/10.3389/fendo.2022.927824
10. Olumide OB, Godwin AI, Titilayo JO, Christian IO, Etukudoh NS, Uchejeso OM, et al. Assessment of Serum Anti-Müllerian Hormone (AMH) as an Independent Marker for Oligozoospermia and Non-Obstructive Azoospermia in Infertile Nigerian Men. Biomedical and Pharmacology Journal. 2023;16(1):35-42. https://doi.org/10.13005/bpj/2585
11. Yuanyuan Z, Guicheng Z, Yi Z, Jiang X. From biological marker to clinical application: the role of anti-Müllerian hormone (AMH) for delayed puberty and idiopathic non-obstructive azoospermia in males. Endocrine connections. 2025; EC-24. https://doi.org/10.1530/EC-24-0630
12. Vannapraseuth B. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction 4th Edition. The Australian Journal of Medical Science. 2005;26:100. https://api.semanticscholar.org/CorpusID:57556090
13. Poulet PE, Tran M, Tezenas du Montcel S, Dubois B, Durrleman S, Jedynak B. Prediction-powered inference for clinical trials. medRxiv. 2025;2001-25. https://doi.org/10.1101/2025.01.15.25320578
14. Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Human Reproduction. 2007;22(1):188-96. https://doi.org/10.1093/humrep/del364
15. Irteimah T, Al Dubais A, Al Rubaihat R. The Impact of Hookah on Anti-mullerian Hormone Level. Journal of the Royal Medical Services. 2022;29(1):28-35. https://doi.org/10.12816/0060310
16. Banihani SA, Shefa'M A. Men with oligozoospermia had lower level of seminal plasma pyridoxine compared to normozoospermic men. Heliyon. 2022;8(12). https://doi.org/10.1016/j.heliyon.2022.e11983
17. Melnyk O V, Vorobets MZ, Fafula R V, Onufrovych OK, Vorobets ZD. Features of spermogram indicators in idiophatic infertility in men. Bulletin of Problems in Biology and Medicine. 2022;167:187-92. https://doi.org/10.29254/2077-4214-2022-4-167-187-192
18. Ahmad SS, Al-Murshidi SY. Evaluation the level of antisperm antibodies, some cytokines and zinc for oligozoospermia, asthenozoospermia patients compared with normozoospermia. International journal of health sciences. 2022;6(S6):5324-31. https://doi.org/10.53730/ijhs.v6nS6.10907
19. Bonanno O, Romeo G, Asero P, Pezzino FM, Castiglione R, Burrello N, et al. Sperm of patients with severe asthenozoospermia show biochemical, molecular and genomic alterations. Reproduction. 2016;152(6):695-704. https://doi.org/10.1530/REP-16-0342
20. Al-Nedaw IA, Hassan SY. A Comparison of ICSI Outcomes and Reactive Oxygen Species Levels in Seminal Plasma between Normozoospermia and Sperm Abnormalities Groups for Infertile Men. Kufa Medical Journal. 2023;19(2). https://doi.org/10.36330/kmj.v19i2.12866
21. Jaber ZA, Mohammed AA, Rahim AI, Technologies AR. Correlation of serum and seminal plasma anti-mullerian hormone with fertility hormones profile and semen parameters. Obstetrics & Gynaecology Forum. 2024;(3):1491-7.
https://obstetricsandgynaecologyforum.com/index.php/ogf/article/view/516
22. Holt R, Yahyavi SK, Kooij I, Andreassen CH, Andersson AM, Juul A, et al. Low serum anti-Müllerian hormone is associated with semen quality in infertile men and not influenced by vitamin D supplementation. BMC Medicine. 2023;21(1):1-10. https://doi.org/10.1186/s12916-023-02782-1
23. Castellini C, Totaro M, Parisi A, D'Andrea S, Lucente L, Cordeschi G, et al. Bisphenol A and male fertility: Myths and realities. Frontiers in endocrinology. 2020;11:540459. https://doi.org/10.3389/fendo.2020.00353
24. Turhan G, Çil N, Kabukçu C, Turan T, Fenkçi İV, Abban MG. Relationship of seminal plasma anti-Müllerian hormone concentration with sperm morphology and sperm DNA damage. Journal of Urological Surgery. 2022; https://doi.org/10.4274/jus.galenos.2022.2021.0121
25. Xiao H, Ding YL, Yang P, Chen Q, Huang HL, Chen X, et al. Association between anti-Müllerian hormone concentrations and sperm retrieval outcomes in patients with idiopathic nonobstructive azoospermia: a systematic review and meta-analysis. Asian Journal of Andrology. 2024;26(5):522-7. https://doi.org/10.4103/aja202419
26. Kang-sheng LIU, Hui YAO, Xiao-dong MAO, Xiao-yong T, Ya-jun C. Application of Anti-Müllerian Hormone in Diagnosis of Male Infertility. Journal of International Translational Medicine. 2017;5(1):19-22.
https://doi.org/10.11910/2227-6394.2017.05.01.04
27. Andersen JM, Herning H, Witczak O, Haugen TB. Anti-Müllerian hormone in seminal plasma and serum: association with sperm count and sperm motility. Human Reproduction. 2016;31(8):1662-7. https://doi.org/10.1093/humrep/dew121
28. Benderradji H, Barbotin AL, Leroy-Billiard M, Prasivoravong J, Marcelli F, Decanter C, et al. Defining reference ranges for serum anti-Müllerian hormone on a large cohort of normozoospermic adult men highlights new potential physiological functions of AMH on FSH secretion and sperm motility. The Journal of clinical endocrinology & metabolism. 2022;107(7):1878-87.
https://doi.org/10.1210/clinem/dgac218
29. Sabir FNK. Association of Anti-Mullerian Hormone with some physiological and immunological parameters of infertile males. Cellular and Molecular Biology. 2022;68(9):171-8. https://doi.org/10.14715/cmb/2022.68.9.27
30. Buratini J, Dellaqua TT, Dal Canto M, La Marca A, Carone D, Mignini Renzini M, et al. The putative roles of FSH and AMH in the regulation of oocyte developmental competence: From fertility prognosis to mechanisms underlying age-related subfertility. Human Reproduction Update. 2022;28(2):232-54. https://doi.org/10.1093/humupd/dmab044
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Osamah A. Layih , Basil O. Saleh

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


