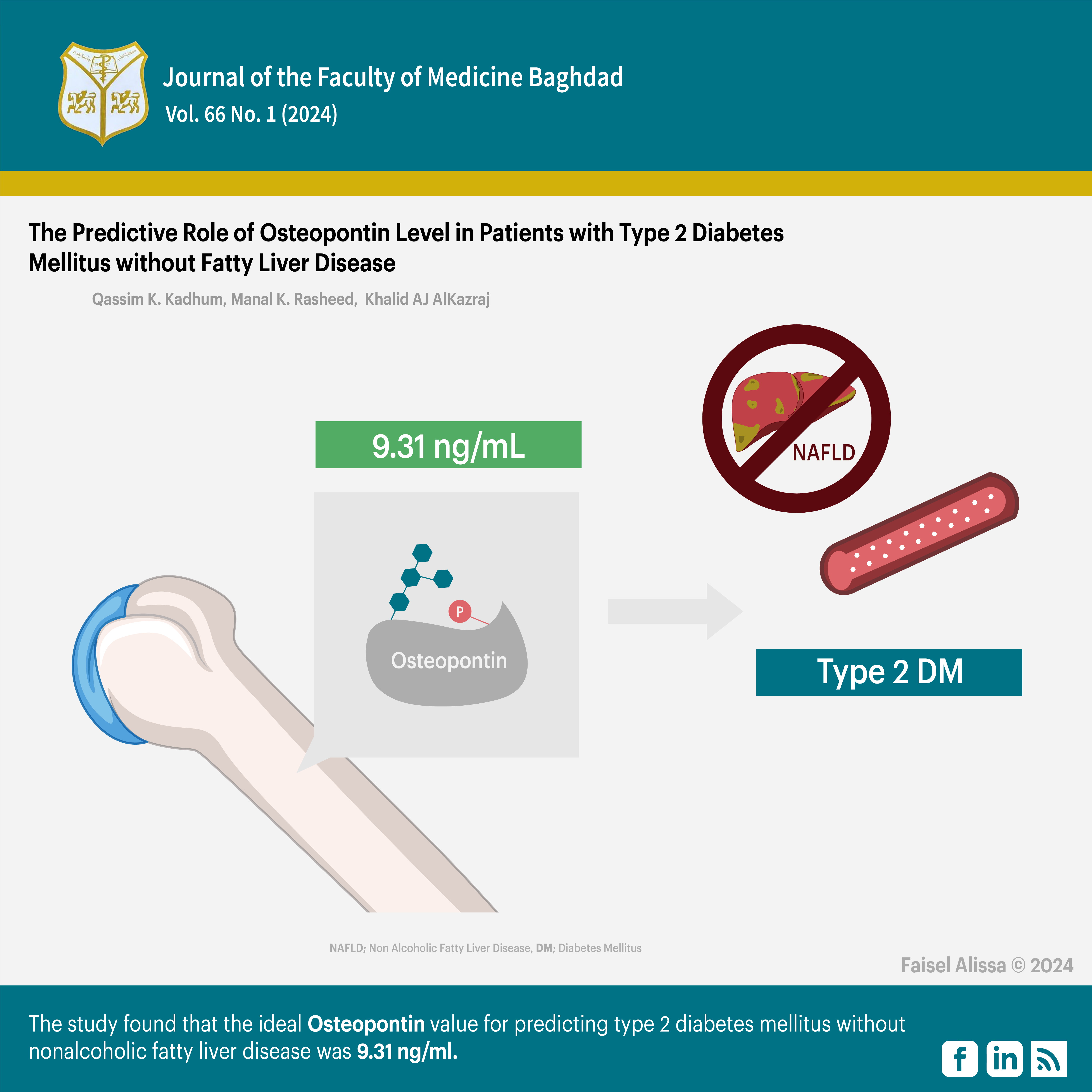
The Predictive Role of Osteopontin Level in Patients with Type 2 Diabetes Mellitus without Fatty Liver Disease
DOI:
https://doi.org/10.32007/jfacmedbagdad.6612182Keywords:
Diabetes mellitus II, Fatty acids, Fatty liver disease, Non-alcoholic, OsteopontinAbstract
Background: Type 2 diabetes mellitus is a condition in which the body is unable to use insulin effectively. This condition was previously known as non-insulin-dependent or adult-onset diabetes. Osteopontin (OPN) is a phosphorylated glycoprotein initially found in a secreted form in bones. Later, it was discovered that it also exists as an intracellular protein.
Objectives: he study aimed to predict Osteopontin levels in type 2 diabetes mellitus patients without fatty liver disease.
Results: The study found that group A had significantly higher levels of FBS, HbA1c, insulin, HOMA-IR, triglycerides, and VLDL compared to group B (P ≤ 0.05). Additionally, group A had significantly lower levels of HDL than group B. However, there were no significant differences in the levels of cholesterol, LDLc, and ALP between the two groups (P ≥ 0.05). The mean ±SD levels of Osteopontin were 23.66 for group A (DM with NAFLD),. 15.65 for group B (DM without NAFLD), and 5.43 for group C (control group ). This indicates a statistically significant difference (P≤0.05) in the mean ±SD levels of Osteopontin among the studied groups.
Conclusion: All parameters are increased in patients with type 2 DM without nonalcoholic fatty liver disease compared to the control group. The recommended threshold for Osteopontin in predicting type 2 diabetes mellitus without non-alcoholic fatty acid liver disease is 9.31 ng/ml.
Received: Aug., 2023
Accepted: Dec., 2023
Published: April, 2024
Downloads
References
World Health Organizattion. Classification of diabetes mellitus: WHO; 2019 Available from: https://www.who.int/publications/i/item/classification-of-diabetesmellitus
Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, Rosas SE, Del Prato S, Mathieu C, Mingrone G, Rossing P. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2022;65(12):1925-66. https://doi.org/10.1007/s00125-022-05787-2
American Diabetes Association. Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021 Jan; 44(Supplement 1): S1-S2 https://doi.org/10.2337/dc21-Sint
American diabetes association .Classification and diagnosis of diabetes sec2 in standards of medical care in diabetes 2016.Diabetes care 2016; 39(supp1.1):s13-s22 https://doi.org/10.2337/dc16-S005
CDC. Centers for disease control and prevention:National Diabetes control and prevention,US: Dept of health and human services 2017.
International Diabetes federation.Diabetes Atlas, Eight edition 2017. https://diabetesatlas.org/
Sangahera DK, Blackett PR.Type2 diabetes genetics beyond GWAS J Diabetes Metab 2012 ;( 198. https://doi.org/10.4172/2155-6156.1000198.
Florez JC.Leveraging genetics to advance type2 DM prevention PLOS medicine 2016; 13(7) el002102. https://doi.org/10.1371/journal.pmed.1002102
O'Regan A, Berman JS. Osteopontin: a key cytokine in cell-mediated and granulomatous inflammation. Int J Exp Pathol. 2000; 81:373-390. https://doi.org/10.1046/j.1365-2613.2000.00163.x
Sodek J, Ganss B, McKee MD. Osteopontin. Crit Rev Oral Biol Med. 2000;11:279-303 https://doi.org/10.1177/10454411000110030101
Berman JS. Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling, and cell survival. J Clin Invest. 2001;107:1055-1061. https://doi.org/10.1172/JCI12980
Abed E, Manal K Rasheed, Khalaf G.Hussein. Assessment of Total Procollagen Type 1 Intact N-terminal Propeptide, C-telopeptide of type 1 collagen, Bone Mineral Density and its Relationship to Body Mass Index in Men with Type 2 Diabetes. JFacMedBagdad [Internet]. 2022. 24 ;64(2):81-5. https://doi.org/10.32007/jfacmedbagdad.6421942 .
Petersen MC, Shulman GI. Mechanisms of Insulin Action and Insulin Resistance. Physiol Rev. 2018;98(4):2133-2223.
https://doi.org/10.1152/physrev.00063.2017
Bermudez V, Salazar J, Martínez MS, Chávez-Castillo M, Olivar LC, Calvo MJ, Palmar J, Bautista J, Ramos E, Cabrera M, Pachano F, Rojas J. Prevalence and Associated Factors of Insulin Resistance in Adults from Maracaibo City, Venezuela. Adv Prev Med. 2016; https://doi.org/10.1155/2016/9405105
Al-Shamma ZA, Al-Yassin HD, Hashim HM. Resistin , Insulin resistance and BMI in type 2 diabetes mellitus and healthy subjects. JFacMedBagdad. 2008; 50(3):377-82. https://doi.org/10.32007/jfacmedbagdad.5031262.
Hammed IK, Abed BA, Rashid NF. Glycated haemoglobin as a dual biomarker Association between HbA1c and dyslipidemia in type 2 diabetic patients. JFacMedBagdad. 2012 54(1):88-92. https://doi.org/10.32007/jfacmedbagdad.541778
Hameed EK, Al-Ameri LT, Hasan HS, Abdulqahar ZH. The Cut-off Values of Triglycerides-Glucose Index for Metabolic Syndrome Associated with Type 2 Diabetes Mellitus. Baghdad Sci. Jour. 2022; 19(2):0340-. https://doi.org/10.21123/bsj.2022.19.2.0340
Okita K, Iwahashi H, Kozawa J, Okauchi Y, Funahashi T, Imagawa A, Shimomura I. Homeostasis model assessment of insulin resistance for evaluating insulin sensitivity in patients with type 2 diabetes on insulin therapy. Endocr J. 2013; 60(3):283-90. https://doi.org/10.1507/endocrj.EJ12-0320
Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K. The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System . Front Immunol. 2020 22; 11:1582https://doi.org/10.3389/fimmu.2020.01582
Fouad SA, Mohamed NA, Fawzy MW, Moustafa DA. Plasma osteopontin level in chronic liver disease and hepatocellular carcinoma. Hepatitis monthly. 2015;15(9). https://doi.org/10.5812/hepatmon.30753
FW, Zeyda M, Gollinger K, Pfau B, Neuhofer A, Weichhart T, Säemann MD, Geyeregger R, Schlederer M, Kenner L, Stulnig TM. Neutralization of osteopontin inhibits obesity-induced inflammation and insulin resistance. Diabetes. 2010; 1; 59(4):935-46. https://doi.org/10.2337/db09-0404
Ramaiah SK, Rittling S. Pathophysiological role of osteopontin in hepatic inflammation, toxicity, and cancer. Toxicological sciences. 2008 May 1; 103(1):4-13.https://doi.org/10.1093/toxsci/kfm246
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes care. 2018; 41(Supplement 1):S13 https://doi.org/10.2337/dc18-S002
Newsholme P, Cruzat V, Arfuso F, Keane K. Nutrient regulation of insulin secretion and action. Journal of Endocrinology. 2014 Jun 1; 221(3):R105-20. https://doi.org/10.1530/JOE-13-06
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, and Turner RC, et al. Homeostasis model assessment: insulin resistance and betacell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 1985; 28:412-419. https://doi.org/10.1007/BF00280883
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gender medicine. 2009 Jan 1;6:60-75..https://doi.org/10.1016/j.genm.2009.02.002
Santos-Gallego CG, Rosenson RS. Role of HDL in those with diabetes. Current cardiology reports. 2014;16:1-4. https://doi.org/10.1007/s11886-014-0512-5
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Qassim AlKenany, Manal Kamal Rasheed, Khalid Abdulla Jasim AlKazraj

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

















 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


