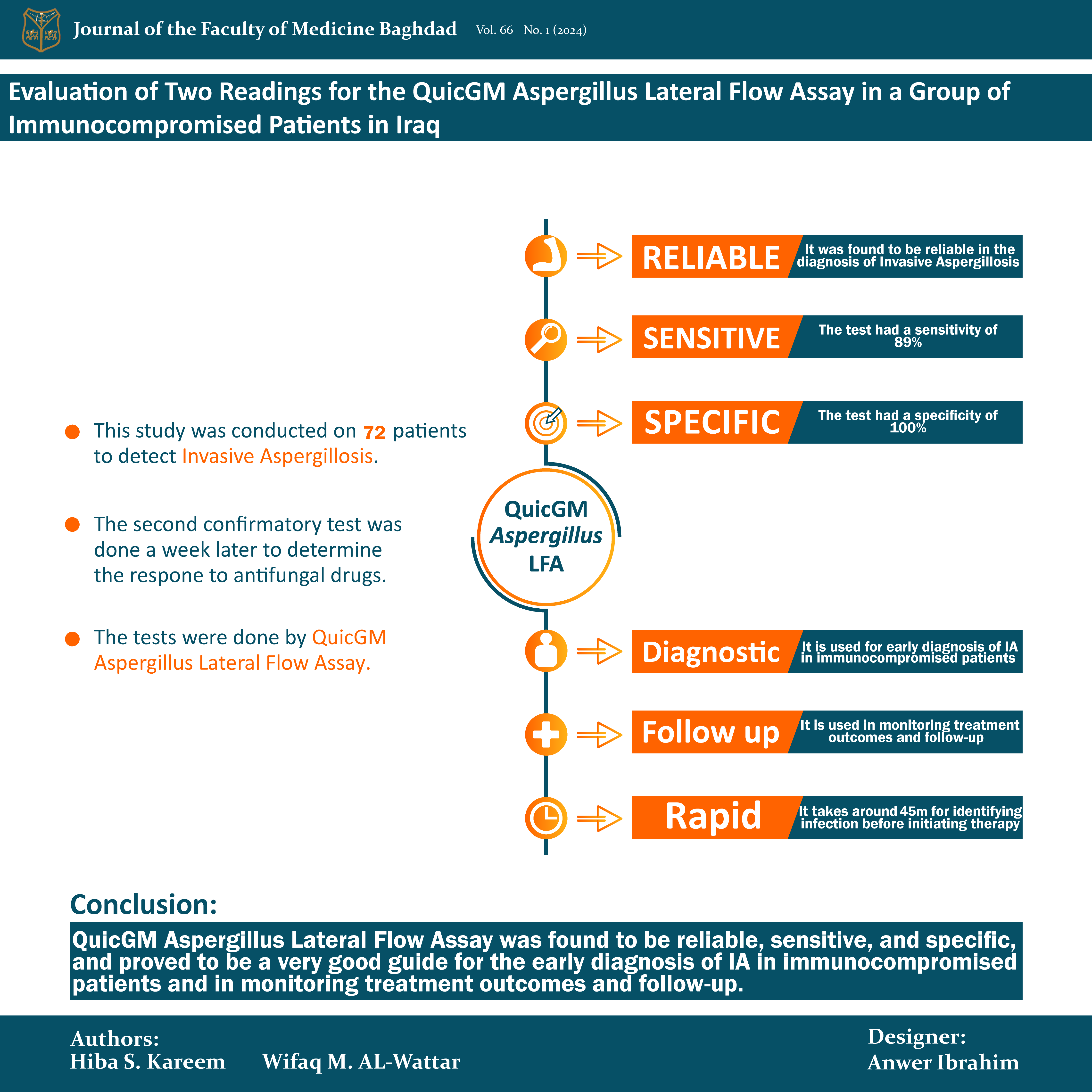
Evaluation of Two Readings for the QuicGM Aspergillus Lateral Flow Assay in a Group of Immunocompromised Patients in Iraq
DOI:
https://doi.org/10.32007/jfacmedbagdad.6622178Keywords:
Aspergillus diagnostics, Galactomannan, Invasive Aspergillosis (IA), Lateral Flow AssayAbstract
Background: Aspergillus spp. causes a wide range of diseases called Invasive Aspergillosis (IA) which is a fatal illness that affects a variety of immunocompromised people worldwide.
Objective: Using the lateral flow test for the detection of Galactomannan antigen in immunocompromised patients suspected to have IA.
Patients and Methods: This study was conducted on 72 patients, whose samples (serum, Bronchoalveolar lavage, Blood) were collected from the Hematology-Oncology Unit at Baghdad Teaching Hospital and Pediatric Welfare Hospital, and ICU in Ghazi AL-Hariri Surgical Specialties Hospital, and Bone Marrow Transplantation Center in period between November 2022 to February 2023. Patients’ blood and sputum were sent for fungal culture to confirm the diagnosis in most cases.
Results: QuicGM Aspergillus Lateral Flow Assay was conducted on 72 patients, of whom 34 () were positive and 38 (52.7) were negative (P-value of 0.001 and 0.5) respectively. This screening aimed at detecting IA. One week later, the second confirmative result was obtained from 24 patients to determine the response to antifungal drugs or recovery from neutropenia on which 15 readings were negative and nine were positive. Out of 48 single readings, 25 were positive and 23 were negative. All for 72 members of the control group gave negative results. This study is the first in Iraq to use this assay.
Conclusion: QuicGM Aspergillus Lateral Flow Assay was found to be reliable, sensitive, and specific, and proved to be a very good guide for the early diagnosis of IA in immunocompromised patients and in monitoring treatment outcomes and follow-up.
Downloads
References
Ledoux MP, Guffroy B, Nivoix Y, Simand C, Herbrecht R. Invasive Pulmonary Aspergillosis. Semin Respir Crit Care Med. 2020; 41(01):080–98. http://doi/10.1055/s-0039-3401990.
Shafiq SA, Al-Joofy AK. Histopathological and enzymatic study on the effect of Aspergillus fumigatus in mice. J Fac Med Baghdad 2010; 52(4). https://doi.org/10.32007/jfacmedbagdad.524962
Mansoor NT, Jalil MJ, Yahya ASM, Abbas LM, Salman MD. Effects of contaminated feed with Aspergillus flavus on some hematological and biochemical parameters on Cyprinus carpio L. 1758. Iraqi J Vet Med. 2018; 42(1):87–91. https://doi.org/10.30539/iraqijvm.v42i1.36
Al-Charrakh AH, Al-Mamory ZO, Al-Malaky KA. Antifungal susceptibility patterns of Aspergillus species isolated from patients with pulmonary diseases in Iraq. J Appl Pharm Sci. 2018; 8(5):088–93. URL
Abomughaid MM. Isolation and identification of fungi from clinical samples of diabetic patients and studying the anti-fungal activity of some natural oils on isolated fungi. Baghdad Sci J. 2021; 18(3):0462–0462. https://doi.org/10.21123/bsj.2021.18.3.0462
Ardi P, Daie-Ghazvini R, Hashemi SJ, Salehi MR, Bakhshi H, Rafat Z, et al. Study on invasive aspergillosis using galactomannan enzyme immunoassay and determining antifungal drug susceptibility among hospitalized patients with hematologic malignancies or candidates for organ transplantation. Microb Pathog. 2020; 147:104382. https://doi.org/10.1016/j.micpath.2020.104382
Aldeen Muhammed MS, Al-Attraqchi AAF, Dawood HN, Hamed Hameed G. Detection of Aspergillus spp. and Candida albicans antigenemia in a sample of Iraqi patients with severe COVID-19. J Emerg Med Trauma Acute Care. 2022; (3). https://doi.org/10.5339/jemtac.2022.ismc.7
Jawad MA, Alkharasani AAH, Zanki FA, AL-Janabi AAHS, Ali RN. Advantages and disadvantages usage of Galactomannan ELISA assay for detection of Aspergillosis. Int J. 2019; 2(6):50. URL
Hsiao HH, Liu YC, Wang HC, Du JS, Tang SH, Yeh TJ, et al. Comparison of a novel lateral-flow device to galactomannan assay at different time periods for detections of invasive aspergillosis. J Formos Med Assoc. 2022; 121(10):2123–9. https://doi.org/10.1016/j.jfma.2022.04.011
Lai G, Zeng C, Mo J, Song W dong, Xu P. Diagnostic Value of Galactomannan in Bronchoalveolar Lavage Fluid for Chronic Respiratory Disease with Pulmonary Aspergillosis. Fenwick B, editor. J Clin Microbiol. 2020 Feb 24; 58(3):e01308-19. https://journals.asm.org/doi/10.1128/JCM.01308-19
Mercier T, Dunbar A, de Kort E, Schauwvlieghe A, Reynders M, Guldentops E, et al. Lateral flow assays for diagnosing invasive pulmonary aspergillosis in adult hematology patients: a comparative multicenter study. Med Mycol . 2020; 58(4):444–52. https://doi.org/10.1093/mmy/myz079
Kindo A. P457 Clinical correlation of beta galactomannan with culture and patient outcome in a tertiary care center in south india. Med Mycol. 2022; 60 (1). https://doi.org/10.1093/mmy/myac072.P457
Aerts R, Mercier T, Maertens J, Lagrou K. P412 QuicGM Aspergillus Galactomannan Ag lateral flow assay as a practical aid to diagnose invasive Aspergillosis in high-risk hematology patients. Med Mycol. 2022; 60(1) 072P412. Available from: URL
Liu C, Peng J, Zhang Y, Wang Y, Wang H, Su Y, et al. P460 The Aspergillus Lateral Flow Assay for the diagnosis of invasive Aspergillosis. Med Mycol 60(1) 072P460. https://doi.org/10.1093/mmy/myac072.P460
Serin I, Dogu MH. Serum Aspergillus galactomannan lateral flow assay for the diagnosis of invasive aspergillosis: A single‐centre study. Mycoses. 2021; 64 (6): 678–83. https://onlinelibrary.wiley.com/doi/10.1111/myc.13265
Jenks JD, Miceli MH, Prattes J, Mercier T, Hoenigl M. The Aspergillus Lateral Flow Assay for the Diagnosis of Invasive Aspergillosis: an Update. Curr Fungal Infect Rep. 2020;14(4):378–83. URL
Aerts R, Cuypers L, Mercier T, Maertens J, Lagrou K. Implementation of Lateral Flow Assays for the Diagnosis of Invasive Aspergillosis in European Hospitals: A Survey from Belgium and a Literature Review of Test Performances in Different Patient Populations. Mycopathologia. 2023; 188(5): 655–65. URL
Priya H, Kothari N, Jain V, Kumar D, Khichar S, Rohila AK, et al. P447 Galactomannan lateral flow assay for the diagnosis of invasive Aspergillosis among clinically suspected patients in tertiary care center, Jodhpur, Rajasthan. Med Mycol. 2022; 60 (1) 46. https://doi.org/10.1093/mmy/myac072.P460
Alhan O, Saba R, Akalin EH, Ener B, Ture Yuce Z, Deveci B, et al. Diagnostic Efficacy of Aspergillus Galactomannan Lateral Flow Assay in Patients with Hematological Malignancies: A Prospective Multicenter Study. Mycopathologia. 2023; 188(5):643–53. URL
Taghavi M, Mortaz E, Nikaein D, Athari S. Significance of galactomannan antigen for Aspergillosis diagnosis: A review. J Mycol Res. 2015; 2(2):111–7. URL
Shariati A, Moradabadi A, Chegini Z, Khoshbayan A, Didehdar M. An Overview of the Management of the Most Important Invasive Fungal Infections in Patients with Blood Malignancies. Infect Drug Resist. 2020; 13:2329–54. URL https://doi.org/10.2147/IDR.S254478
Ali R, AL-Wattar WMA, Jawad AM. Detection of Galactomannan Antigen in the Serum of Iraqi Patients with Suspected Invasive Aspergillosis. J Fac Med Baghdad. 2016; 58(1):71–4. https://doi.org/10.32007/jfacmedbagdad.581200
Al-Wattar WMA. Overview on common fungal infections, recovered in Baghdad teaching hospitals in five years. Iraq Med J. 2020;4(2). https://doi.org/10.22317/imj.v4i2.819
Al-Rawazq HS, Mohammed AK, Al-Zubaidy RH. Bacterial Isolates in Blood Culture of Children with Septicemia. J Fac Med Baghdad. 2012; 54(1):96–9. https://doi.org/10.32007/jfacmedbagdad.541781
Sato S, Kamata W, Fukaguchi K, Tsunoda S, Kamio T, Koyama H, et al. Successful treatment of invasive tracheobronchial pulmonary aspergillosis with venovenous extracorporeal membrane oxygenation and combined systemic, intratracheal instillation of liposomal amphotericin B: a case report. J Med Case Reports . 2022 16(1):470.URL
Al-Watar WMA, Al-Fakar SA, Mohammed KIA, Ali SHM. Anti Fungal Resistance of Some Yeasts Recovered in a Group of Immuno Compromised Patients. URL
Tunccan OG, Aki SZ, Akyurek N, Sucak G, Senol E. Isolated cutaneous aspergillosis in an acute lymphoblastic leukemia patient after allogeneic stem cell transplantation. J Infect Dev Ctries. 2011; 5(05):406–9. https://doi.org/10.3855/jidc.1466
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Hiba S. Kareem, Wifaq M. Al-Wattar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Permit others to copy and distribute the manuscript; to extract, revise, and create another derivative
works of or from the manuscript (e.g., a translation); to incorporate the manuscript into a
collective work; and to text or data mine the article, even for commercial purposes, provided that
the author(s) is/are credited; the article's modifications should not harm the author's honor or
reputation; and the article should not be altered in a way that would cause the author to lose them
reputation. The Creative Commons Attribution 4.0 International License (CC BY 4.0) has more
information.
















 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..


